Topics :
Latest Post
Showing posts with label treatment. Show all posts
Showing posts with label treatment. Show all posts
12:28 AM
How Is Mesothelioma Diagnosed?
How Is Mesothelioma Diagnosed?
 how is Mesothelioma Diagnosed?
how is Mesothelioma Diagnosed?
Diagnosing mesothelioma can be difficult since there's loads of conditions that cause similar signs. Your physician will first take a cautious history, questioning you about your employment history, and then perform a physical examination. Imaging studies are often done, and may include x-rays of your chest and abdomen, CT scans, MRI scans or PET scans.
* Localized (Stage 1) – With localized mesothelioma, the cancer is confined to the mesothelium – the pleura with pleural mesothelioma, or the peritoneum with peritoneal mesothelioma
* Advanced (Stage 2, 3, and 4) – Mesothelioma is thought about advanced if it's spread to the lymph nodes, or other organs including the lungs
What am I able to Do to Prevent Mesothelioma?
The most important thing you can do to prevent mesothelioma is to make use of appropriate precautions in the event you are exposed to asbestos at work. OSHA has asbestos safety standards for individuals who may be exposed on the job. in the event you work with asbestos, it is important to follow these guidelines to minimize your families exposure as well. Asbestos insulation in homes is usually not an issue, unless it is damaged or disturbed by remodeling projects. in the event you may have asbestos insulation (homes built prior to 1950) make sure to hire a contractor certified in asbestos management before you start any home improvement projects.
How is Mesothelioma Treated?
Depending on the size and destination of your tumor, and if it's spread, treatment options may include:
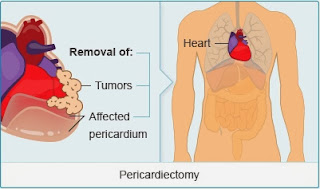
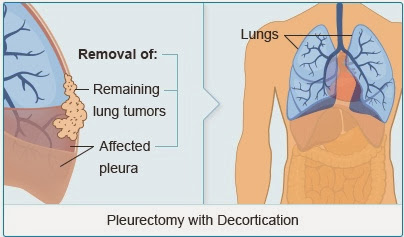
* Surgery – Surgery may be thought about, if the tumor is caught at an early stage. Types of surgery include:
o Pleurectomy – With a pleurectomy, a portion of the pleura is removed
o Extrapleural pneumonectomy – A portion of the pleura is removed, and a portion of the pericardium (heart lining), diaphragm (muscle separating the chest and abdomen) and the lung
* Chemotherapy – a mix of a chemotherapy medication and a targeted therapy may improve survival.
* Radiation Therapy – Radiation therapy is occasionally used as a palliative treatment for mesothelioma, a treatment that does not cure cancer, but can make you more comfortable. It may also be used after surgery to kill any remaining cancer cells.
* Clinical Trials – Several clinical trials are in progress, evaluating new ways to treat mesothelioma.
Living With Mesothelioma
On top of the heartbreak a diagnosis of cancer brings, plenty of people with mesothelioma lack the emotional and psychosocial support that those with other forms of cancer find available. In addition, medico-legal battles related to asbestos exposure on-the-job can be emotionally draining. Participating in a support group, either through your cancer center, community, or online, can help you wade through the maze of treatment options, and find camaraderie in others who are living with mesothelioma.
If your doctor suspects mesothelioma, he will need to schedule a biopsy.
Depending upon the destination of your tumor, he may recommend a
thoracoscopy or video-assisted thoracoscopy (VAT), a procedure where a
tissue sample is taken from the pleura, or a peritoneoscopy, a similar
procedure to receive tissue from the abdomen. If the biopsy reveals
mesothelioma, further studies are then done to decide the stage of the
cancer (how advanced it is).
Stages of Mesothelioma
Mesothelioma is divided in to 2 primary stages:
Stages of Mesothelioma
Mesothelioma is divided in to 2 primary stages:
 how is Mesothelioma Diagnosed?
how is Mesothelioma Diagnosed?Diagnosing mesothelioma can be difficult since there's loads of conditions that cause similar signs. Your physician will first take a cautious history, questioning you about your employment history, and then perform a physical examination. Imaging studies are often done, and may include x-rays of your chest and abdomen, CT scans, MRI scans or PET scans.
* Localized (Stage 1) – With localized mesothelioma, the cancer is confined to the mesothelium – the pleura with pleural mesothelioma, or the peritoneum with peritoneal mesothelioma
* Advanced (Stage 2, 3, and 4) – Mesothelioma is thought about advanced if it's spread to the lymph nodes, or other organs including the lungs
What am I able to Do to Prevent Mesothelioma?
The most important thing you can do to prevent mesothelioma is to make use of appropriate precautions in the event you are exposed to asbestos at work. OSHA has asbestos safety standards for individuals who may be exposed on the job. in the event you work with asbestos, it is important to follow these guidelines to minimize your families exposure as well. Asbestos insulation in homes is usually not an issue, unless it is damaged or disturbed by remodeling projects. in the event you may have asbestos insulation (homes built prior to 1950) make sure to hire a contractor certified in asbestos management before you start any home improvement projects.
How is Mesothelioma Treated?
Depending on the size and destination of your tumor, and if it's spread, treatment options may include:
* Surgery – Surgery may be thought about, if the tumor is caught at an early stage. Types of surgery include:
o Pleurectomy – With a pleurectomy, a portion of the pleura is removed
o Extrapleural pneumonectomy – A portion of the pleura is removed, and a portion of the pericardium (heart lining), diaphragm (muscle separating the chest and abdomen) and the lung
* Chemotherapy – a mix of a chemotherapy medication and a targeted therapy may improve survival.
* Radiation Therapy – Radiation therapy is occasionally used as a palliative treatment for mesothelioma, a treatment that does not cure cancer, but can make you more comfortable. It may also be used after surgery to kill any remaining cancer cells.
* Clinical Trials – Several clinical trials are in progress, evaluating new ways to treat mesothelioma.
Living With Mesothelioma
On top of the heartbreak a diagnosis of cancer brings, plenty of people with mesothelioma lack the emotional and psychosocial support that those with other forms of cancer find available. In addition, medico-legal battles related to asbestos exposure on-the-job can be emotionally draining. Participating in a support group, either through your cancer center, community, or online, can help you wade through the maze of treatment options, and find camaraderie in others who are living with mesothelioma.
By: hehhe
Labels:
Mesothelioma,
treatment
11:53 PM
A Basic Guide To Recognizing And Treating Mesothelioma
A Basic Guide To Recognizing And Treating Mesothelioma
The average life span of a person diagnosed with the disease is about 4 to 24 months from the finding. About 3,000 people in the U.S. die of mesothelioma every year. People at risk are those who have been previously exposed to asbestos dust, including former steel workers, auto mechanics, mineworkers, and military workers, among many others. Their family members may also be at risk, as the asbestos dust from clothing can travel through the air.
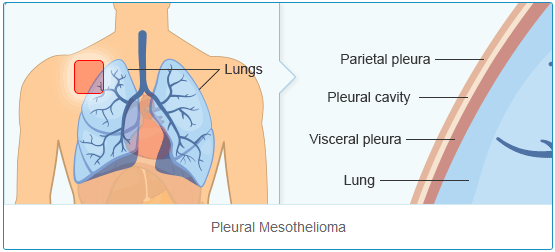
Mesothelioma is a rare form of cancer that is usually found in those
previously exposed to asbestos. Cancerous cells form in the mesothelium,
which is a protective lining that covers most of the body's internal
organs. These cells typically form in the lining of the lungs, abdomen,
or the sac that encircles the heart.
The average life span of a person diagnosed with the disease is about 4 to 24 months from the finding. About 3,000 people in the U.S. die of mesothelioma every year. People at risk are those who have been previously exposed to asbestos dust, including former steel workers, auto mechanics, mineworkers, and military workers, among many others. Their family members may also be at risk, as the asbestos dust from clothing can travel through the air.
Mesothelioma has an extremely long latency period, which means that
symptoms of the disease may not emerge until 30 to 50 years after the
initial exposure to asbestos. Pleural mesothelioma, which is the most
common type and affects the area around the lungs, may cause shortness
of breath, chest pains, and a persistent cough, which may lead to
coughing up blood. These symptoms are caused by the build up of fluid
between the lining of the lung and the chest cavity. The disease may
start in the chest area and spread to other areas of the body. Other
symptoms of pleural mesothelioma include weight loss, severe breathing
trouble, fever, difficulty swallowing, and swelling of the face and neck
areas. It should be noted that some people with the disease do not
experience any serious symptoms at all.
Peritoneal mesothelioma is rarer than pleural mesothelioma, and affects the abdominal area. Symptoms of peritoneal mesothelioma include abdominal swelling and pain due to the build up of fluid in the abdominal cavity, nausea, loss of appetite, and vomiting. Breathing complications and chest pains may also be present, as well as bowel obstruction, anaemia, fever, and blood clotting.
The rarest form of the disease is pericardial mesothelioma, which first forms in the area surrounding the heart. Tumors grow in the tissues around the heart and spread from there. Chest pain, shortness of breath, constant coughing, and shivering may be symptoms of this form of mesothelioma.
Diagnosis of the disease is oftentimes difficult, due to the fact that the symptoms associated with mesothelioma are similar to those of other conditions. The symptoms of the disease become more serious as the cancerous tumors enter the later stages of development, so people who have been exposed to asbestos at any time in their lives should contact their doctor immediately. Even if a person has never been exposed directly to asbestos but is experiencing any of the above symptoms, they should inform their doctor as soon as possible, as asbestos dust and fibres may have traveled through the air from items such as clothing.
People who have been diagnosed with any form of mesothelioma should immediately contact a lawyer. Individual states have their own statutes of limitation, meaning that there is a set time limit regarding how long a patient has to act on their diagnosis. When searching for a lawyer to handle your case, be sure to find one that has prior experience with mesothelioma cases. They will have the contacts and resources to take care of your case in a timely manner. The Internet is a helpful and efficient resource for a mesothelioma lawyer search.
Patients do not have to be concerned with paying lawyers up-front, since the majority of mesothelioma lawyers work on a contingency fee basis, which means that they will not request payment of any kind unless they successfully settle your case. Lawyers will usually take a 35% cut of whatever settlement or reward the patient receives, but patients seeking compensation for their disease have nothing to lose and everything to gain in going to a lawyer for help.
The average mesothelioma-related settlement in the U.S. is $1 million. Cases that go to trial average awards of approximately $6 million, according to the RAND Corporation. A bill called the Fairness in Asbestos Injury Resolution Act of 2005 (FAIR Act of 2005) introduced on March 17, 2005, seeks to create set amounts of compensation for mesothelioma victims, which would depend on their symptoms.
People who have mesothelioma are able to seek large compensation amounts because their disease is a result of a company's decision not to take sufficient measures to protect its workers from breathing in asbestos while on the job.
Peritoneal mesothelioma is rarer than pleural mesothelioma, and affects the abdominal area. Symptoms of peritoneal mesothelioma include abdominal swelling and pain due to the build up of fluid in the abdominal cavity, nausea, loss of appetite, and vomiting. Breathing complications and chest pains may also be present, as well as bowel obstruction, anaemia, fever, and blood clotting.
The rarest form of the disease is pericardial mesothelioma, which first forms in the area surrounding the heart. Tumors grow in the tissues around the heart and spread from there. Chest pain, shortness of breath, constant coughing, and shivering may be symptoms of this form of mesothelioma.
Diagnosis of the disease is oftentimes difficult, due to the fact that the symptoms associated with mesothelioma are similar to those of other conditions. The symptoms of the disease become more serious as the cancerous tumors enter the later stages of development, so people who have been exposed to asbestos at any time in their lives should contact their doctor immediately. Even if a person has never been exposed directly to asbestos but is experiencing any of the above symptoms, they should inform their doctor as soon as possible, as asbestos dust and fibres may have traveled through the air from items such as clothing.
People who have been diagnosed with any form of mesothelioma should immediately contact a lawyer. Individual states have their own statutes of limitation, meaning that there is a set time limit regarding how long a patient has to act on their diagnosis. When searching for a lawyer to handle your case, be sure to find one that has prior experience with mesothelioma cases. They will have the contacts and resources to take care of your case in a timely manner. The Internet is a helpful and efficient resource for a mesothelioma lawyer search.
Patients do not have to be concerned with paying lawyers up-front, since the majority of mesothelioma lawyers work on a contingency fee basis, which means that they will not request payment of any kind unless they successfully settle your case. Lawyers will usually take a 35% cut of whatever settlement or reward the patient receives, but patients seeking compensation for their disease have nothing to lose and everything to gain in going to a lawyer for help.
The average mesothelioma-related settlement in the U.S. is $1 million. Cases that go to trial average awards of approximately $6 million, according to the RAND Corporation. A bill called the Fairness in Asbestos Injury Resolution Act of 2005 (FAIR Act of 2005) introduced on March 17, 2005, seeks to create set amounts of compensation for mesothelioma victims, which would depend on their symptoms.
People who have mesothelioma are able to seek large compensation amounts because their disease is a result of a company's decision not to take sufficient measures to protect its workers from breathing in asbestos while on the job.
By: Ray Good
Labels:
Mesothelioma,
treatment
2:15 AM
A Guide To The Forms Of Mesothelioma Treatment
A Guide To The Forms Of Mesothelioma Treatment
 Types of Mesothelioma Treatment
Types of Mesothelioma Treatment
Mesothelioma treatment options available today are radiation, chemotherapy, radical surgery and/or combination of all these treatments. During surgery, either a part of tumor or the whole tumor is removed. In some cases, a portion of the normal tissue surrounding the area is also removed along with the tumor.
Mesothelioma treatment, in which the doctors try to cure the patient with drugs, is known as chemotherapy. As the mesothelioma cancer is a rare disease, very little information is available regarding the effects of different drugs on different patients. Adriamycm, (doxorubicin), Cytoxan, (cyclophosphamide), 5-fluorouracil and 5-azacytidine are some of the drugs that have shown good results and a response rate of 0 to 35 % when tried on mesothelioma patients. Some other effective drugs for mesothelioma treatment are cisplatin, high dose methotrexate, interferon, anthracycline analogues and vinblastine. The National Cancer Institute is sponsoring further studies the effectiveness of these and other drugs by funding many clinical centers.
Radiation is another option of mesothelioma treatment that is more helpful in reducing the pain rather than curing the disease itself. Because of the severity of the disease, standard dose of 6,000 rads of radiation has very little effect on mesothelioma patients. In limited cases, some benefit is observed when patient is treated with aggressive high dose radiation. Use of radioactive compounds on diseased tissue has also shown some positive results with the individuals diagnosed early on. Patients of pleural mesothelioma survived for over 24 months when radioactive colloidal gold (Au 198) was placed between the two pleural membranes. Scientists are hopeful that radioactive chromic phosphate, p32 can be used as an effective mesothelioma treatment. This might increase the survival period of patients suffering from peritoneal mesothelioma.
Like the treatment of other cancers, mesothelioma treatment also has its side effects. Nausea and vomiting are some minor problems associated with radiation therapy and chemotherapy that could be controlled with medicines. However, suppression of bone marrow is a serious short-term side effect that may cause WBC, RBC and platelets counts to go down. Such patients may become susceptible to bleeding and infection and may require antibiotic therapy or any other supportive care.
Mesothelioma treatment can be a very expensive and lengthy procedure. However, the patients suffering from mesothelioma cancers can seek compensation for mesothelioma treatments. They can file lawsuits against the individuals or organizations responsible for causing asbestos exposure.
Mesothelioma treatment relates relieving or curing the deadly disease
called mesothelioma. Mesothelioma is serious disease that affects the
lining of lungs, abdominal organs or heart. Mesothelioma can be of two
types, either benign or malignant. Mesothelioma treatment, for an
individual suffering from benign mesothelioma, is surgery. However, in
case of malignant mesothelioma scientists could not find any established
mesothelioma treatment to cure the patient fully.
 Types of Mesothelioma Treatment
Types of Mesothelioma TreatmentMesothelioma treatment options available today are radiation, chemotherapy, radical surgery and/or combination of all these treatments. During surgery, either a part of tumor or the whole tumor is removed. In some cases, a portion of the normal tissue surrounding the area is also removed along with the tumor.
Mesothelioma treatment, in which the doctors try to cure the patient with drugs, is known as chemotherapy. As the mesothelioma cancer is a rare disease, very little information is available regarding the effects of different drugs on different patients. Adriamycm, (doxorubicin), Cytoxan, (cyclophosphamide), 5-fluorouracil and 5-azacytidine are some of the drugs that have shown good results and a response rate of 0 to 35 % when tried on mesothelioma patients. Some other effective drugs for mesothelioma treatment are cisplatin, high dose methotrexate, interferon, anthracycline analogues and vinblastine. The National Cancer Institute is sponsoring further studies the effectiveness of these and other drugs by funding many clinical centers.
Radiation is another option of mesothelioma treatment that is more helpful in reducing the pain rather than curing the disease itself. Because of the severity of the disease, standard dose of 6,000 rads of radiation has very little effect on mesothelioma patients. In limited cases, some benefit is observed when patient is treated with aggressive high dose radiation. Use of radioactive compounds on diseased tissue has also shown some positive results with the individuals diagnosed early on. Patients of pleural mesothelioma survived for over 24 months when radioactive colloidal gold (Au 198) was placed between the two pleural membranes. Scientists are hopeful that radioactive chromic phosphate, p32 can be used as an effective mesothelioma treatment. This might increase the survival period of patients suffering from peritoneal mesothelioma.
Like the treatment of other cancers, mesothelioma treatment also has its side effects. Nausea and vomiting are some minor problems associated with radiation therapy and chemotherapy that could be controlled with medicines. However, suppression of bone marrow is a serious short-term side effect that may cause WBC, RBC and platelets counts to go down. Such patients may become susceptible to bleeding and infection and may require antibiotic therapy or any other supportive care.
Mesothelioma treatment can be a very expensive and lengthy procedure. However, the patients suffering from mesothelioma cancers can seek compensation for mesothelioma treatments. They can file lawsuits against the individuals or organizations responsible for causing asbestos exposure.
By: Ray Good
Labels:
Mesothelioma,
treatment
1:24 AM
Curing Mesothelioma - Can It Be Done?
Curing Mesothelioma - Can It Be Done?
With the likehood of cure for mesothelioma , traditional methods were
not capable of new forms of treatment for mesothelioma have been studied
and studied to provide. Mesothelioma experts are optimistic that new
and effective ways to treat this rare type of cancer will soon be the
victims of the disease caused by asbestos disposal.
Some of the studies
currently underway are: Anti-angiogenesis, this method is the use of special drugs that prevent
tumor growth by building the blood vessels. Unlike other
anti-angiogenesis cancer cells directly, but affects the blood supply is
crucial for the survival and growth of existing tumors and the
development of new ones.
Photodynamic therapy (PDT), there is a recent method that has specialized in the treatment of pleural mesothelioma. However, studies reveal that patients with metastatic mesothelioma not responded to Paris, while a number of encouraging results for patients with moderate disease that has not widen yet. With energy from light, PDT can go to destroy cancer cells.
Immunotherapy , as well called biological therapy. This method is specific for the body's immune system strengthened in the fight against cancer. The immune system plays an important role in the fight against all forms of cancer. But particularly for mesothelioma, where normal methods of treatment is not a cure, study is hope that immunotherapy may be the next big breakthrough in the treatment of this health condition with asbestos be rare here.
Immunotherapy for mesothelioma can be divided into two main categories:
A. Active immunotherapy - in this process are cancer cells from the patients away, and then analyzed in a laboratory, a vaccine that can go back to the sacrifice of mesothelioma in order to be fed to the theory and not develop-scientific The immune system recognizes the vaccine as a threat and then do the same with regard to the actual cancer cells.
B. Passive immunotherapy is in this process, substances such as cytokines or related items to the body's immune system in terms of how it reacts to affect cancer cells.
Gene therapy is the method of genetic target cancer cells and enhance their actual sensitivity to chemotherapeutic agents. One of the most promising of a new gene therapy treatment of mesothelioma is called "suicide gene therapy." Basically forces cancer cells to commit suicide.
All new mesothelioma treatments are at this time only mentioned in clinical studies in patients who are interested.
Photodynamic therapy (PDT), there is a recent method that has specialized in the treatment of pleural mesothelioma. However, studies reveal that patients with metastatic mesothelioma not responded to Paris, while a number of encouraging results for patients with moderate disease that has not widen yet. With energy from light, PDT can go to destroy cancer cells.
Immunotherapy , as well called biological therapy. This method is specific for the body's immune system strengthened in the fight against cancer. The immune system plays an important role in the fight against all forms of cancer. But particularly for mesothelioma, where normal methods of treatment is not a cure, study is hope that immunotherapy may be the next big breakthrough in the treatment of this health condition with asbestos be rare here.
Immunotherapy for mesothelioma can be divided into two main categories:
A. Active immunotherapy - in this process are cancer cells from the patients away, and then analyzed in a laboratory, a vaccine that can go back to the sacrifice of mesothelioma in order to be fed to the theory and not develop-scientific The immune system recognizes the vaccine as a threat and then do the same with regard to the actual cancer cells.
B. Passive immunotherapy is in this process, substances such as cytokines or related items to the body's immune system in terms of how it reacts to affect cancer cells.
Gene therapy is the method of genetic target cancer cells and enhance their actual sensitivity to chemotherapeutic agents. One of the most promising of a new gene therapy treatment of mesothelioma is called "suicide gene therapy." Basically forces cancer cells to commit suicide.
All new mesothelioma treatments are at this time only mentioned in clinical studies in patients who are interested.
By: Dona Kiyo
Labels:
Mesothelioma,
treatment
9:23 PM
Criteria That Are Sufficient To Identify Mesothelioma With High Specificity
Criteria That Are Sufficient To Identify Mesothelioma With High Specificity
One study is called, “Immunohistochemical reactivity in mesothelioma and
adenocarcinoma: A stepwise logistic regression analysis” by Annika
Dejmek, Anders Hjerpe - 1994 Acta Pathologica, Microbiologica et
Immunologica Scandinavica – APMIS Volume 102, Issue 1-6, pages 255–264,
January 1994. Here is an excerpt: “Histological sections from 103
malignant mesotheliomas and 43 adenocarcinoma metastases in pleural
biopsies were investigated for reactivity against a panel of 11
different antibodies. The size of the material allowed the evaluation by
stepwise logistic regression analysis, which selected five parameters
of major importance: vimentin reactivity in epithelial cells, reactivity
to low-molecular-weight keratins in fibrous cells, strong membrane
accentuation of EM A reactivity, and lack of reactivity to LeuM1 and
BerEp4.
Three of these criteria were sufficient to identify a
mesothelioma with high specificity and with a sensitivity of
approximately 70%. Whilst the monoclonal anti-CEA tested was the most
valuable single parameter, it did not add any diagnostic information to
the combination of criteria selected by the stepwise logistic regression
analysis. However, this antibody can be used to exclude most of the
adenocarcinomas from further analysis with the more extensive panel.”
Another study is called, “Ectopic thymoma mimicking diffuse pleural
mesothelioma: A case report” - Volume 29, Issue 4, Pages 409-410 (April
1998) by Hiroaki Fushimi, MD, Yoshiro Tanio, MD, Kiyoshi Kotoh, MD. Here
is an excerpt: “Abstract - A case of ectopic thymoma of the pleura with
a particular growth pattern mimicking diffuse pleural mesothelioma is
reported. Diagnostic imaging showed that the pleural tumor encased the
entire left lung.
The specimen biopsied from the tumor was composed of
lymphocytes and epithelial cells, consistent with the mixed type of
thymoma. The autopsy found no evidence of a mediastinal tumor. An
involuted thymus was found in the parietal pleural tissue adhered to the
apex of the left lung. The thymoma was thought to originate from the
ectopic thymic tissue in the parietal pleura, as a lesion independent
from the primary mediastinal thymoma, and spread along the pleura like
diffuse mesothelioma.
Another study is called, “Dose-Dependent Pulmonary Toxicity After
Postoperative Intensity-Modulated Radiotherapy for Malignant Pleural
MesotheliomaPresented at the 48th Annual Meeting of the American Society
for Therapeutic and Radiation Oncology (ASTRO), Philadelphia, PA,
November 5–9, 2006. - International Journal of Radiation Oncology
Biology Physics - Volume 69, Issue 2 , Pages 350-357, 1 October 2007 by David C. Rice, M.B., B.Ch. Affiliations - Department of Thoracic and
Cardiovascular Surgery, The University of Texas M. D. Anderson Cancer
Center, Houston, TX. Here is an excerpt: “Purpose: To determine the
incidence of fatal pulmonary events after extrapleural pneumonectomy and
hemithoracic intensity-modulated radiotherapy (IMRT) for malignant
pleural mesothelioma. Methods and Materials: We retrospectively reviewed
the records of 63 consecutive patients with malignant pleural
mesothelioma who underwent extrapleural pneumonectomy and IMRT at the
University of Texas M. D. Anderson Cancer Center. The endpoints studied
were pulmonary-related death (PRD) and non–cancer-related death within 6
months of IMRT.
Results: Of the 63 patients, 23 (37%) had died within 6 months of IMRT
(10 of recurrent cancer, 6 of pulmonary causes [pneumonia in 4 and
pneumonitis in 2], and 7 of other noncancer causes [pulmonary embolus in
2, sepsis after bronchopleural fistula in 1, and cause unknown but
without pulmonary symptoms or recurrent disease in 4]). On univariate
analysis, the factors that predicted for PRD were a lower preoperative
ejection fraction (p = 0.021), absolute volume of lung spared at 10 Gy
(p = 0.025), percentage of lung volume receiving e20 Gy (V20; p =
0.002), and mean lung dose (p = 0.013). On multivariate analysis, only
V20 was predictive of PRD (p = 0.017; odds ratio, 1.50; 95% confidence
interval, 1.08–2.08) or non–cancer-related death (p = 0.033; odds ratio,
1.21; 95% confidence interval, 1.02–1.45).
Conclusion: The results of our study have shown that fatal pulmonary
toxicities were associated with radiation to the contralateral lung. V20
was the only independent determinant for risk of PRD or
non–cancer-related death. The mean V20 of the non-PRD patients was
considerably lower than that accepted during standard thoracic
radiotherapy, implying that the V20 should be kept as low as possible
after extrapleural pneumonectomy.
Labels:
Mesothelioma,
treatment
12:04 AM
Demonstrating The Feasibility Of Intrapleural Cisplatin-based Chemotherapy
Demonstrating The Feasibility Of Intrapleural Cisplatin-based Chemotherapy
One interesting study is called, “Trials in malignant mesothelioma. LCSG 851 and 882. Rusch VW” - Chest. 1994 December 106 (6 Suppl) : 359S-362S - Thoracic Surgery Service, Memorial Sloan-Kettering Cancer Center, New York 10021.
Here is an excerpt: “Abstract - In 1985 the Lung Cancer Study Group (LCSG) initiated clinical trials in malignant pleural mesothelioma because LCSG member institutions had access to large numbers of patients and had significant experience treating this uncommon cancer.
The first trial, LCSG 851, defined the patient population seen by the LCSG, and the feasibility of performing surgical resection by extrapleural pneumonectomy in a multi-institutional setting. Of 83 patients entered on this study from September 1985 to June 1988, only 20 could undergo an extrapleural pneumonectomy, and 3 of 20 patients died postoperatively.
This experience prompted the LCSG to explore combining a potentially less morbid operation, pleurectomy/decortication, with adjuvant therapy. The results of another LCSG trial (LCSG 861) and of a small single institutional pilot study demonstrated the feasibility of intrapleural cisplatin-based chemotherapy, and led to the development of LCSG 882, which combined pleurectomy/decortication with postoperative intrapleural, and subsequent systemic, cisplatin-based chemotherapy.
This study was not completed because of discontinuation of funding for the LCSG. However, a single-institution phase 2 trial of very similar design has subsequently shown the feasibility of this combined modality approach.”
Another study is called, “Extended Surgical Staging for Potentially Resectable Malignant Pleural Mesothelioma” by David C. Rice, MB, BCh, Jeremy J. Erasmus, MD, Craig W. Stevens, MD, PhD, Ara A. Vaporciyan, MD, Judy S. Wu, BS, Anne S. Tsao, MD, Garrett L. Walsh, MD, Stephen G. Swisher, MD, Wayne L. Hofstetter, MD, Nelson G. Ordonez, MD, W. Roy Smythe, MD - Ann Thorac Surg 2005;80:1988-1993 - Department of Thoracic and Cardiovascular Surgery, The University of Texas M.D. Anderson Cancer Center, Houston, Texas.
Here is an excerpt: “BACKGROUND: Extrapleural pneumonectomy for malignant pleural mesothelioma (MPM) is a high-risk procedure, and patients require careful preoperative staging to exclude advanced disease. Computed tomography, magnetic resonance imaging, and positron emission tomography are useful staging modalities, but do not reliably identify contralateral mediastinal involvement or transdiaphragmatic invasion. We evaluated the role of extended surgical staging procedures, which generally includes a combination of laparoscopy, peritoneal lavage, and mediastinoscopy, to more precisely stage patients with MPM.
METHODS: One hundred eighteen patients with MPM, deemed clinically and radiologically resectable, underwent extended surgical staging. Mediastinoscopy was performed in 111 patients, laparoscopy in 109 patients, and peritoneal lavage in 78 patients.
RESULTS: Ten (9.2%) patients had gross evidence of transdiaphragmatic or peritoneal involvement. Peritoneal lavage was positive for metastatic MPM in 2 (2.6%) patients, neither of whom had obvious transdiaphragmatic invasion. Ipsilateral mediastinal nodes contained metastatic tumor in 10 of 62 (16.1%) patients. Contralateral nodes were positive in 4 of 111 (3.6%) patients. Of the patients who underwent biopsy of both ipsilateral and contralateral mediastinal nodes, and who had complete pathologic staging after extrapleural pneumonectomy (n = 46), 14 (30.4%) had N2-positive nodes.
Only 5 of these patients were correctly identified by mediastinoscopy (sensitivity 36%, accuracy 80%). Extended surgical staging identified 16 (13.6%) patients who had contralateral nodal involvement, transdiaphragmatic invasion, or positive peritoneal cytology.
CONCLUSIONS: Extended surgical staging defines an important subset of patients with unresectable MPM not identified by imaging. Because of the potential morbidity associated with extrapleural pneumonectomy, we advocate that extended surgical staging be performed in all patients with MPM before resection.
Another interesting study is called, “Phase II study of a short course of weekly high-dose cisplatin combined with long-term oral etoposide in pleural Mesothelioma” - Oxford Journals Medicine Annals of Oncology Volume 6, Issue 6 Pp. 613-616 - A. S. T. Planting1, M. E. L. van der Burg, S. H. Goey, J. H. M. ScheUens, M. J. van den Bent, M. de Boer-Dennert, G. Stoter1 and J. Verweij.
Here is an excerpt: “Abstract - Background In a previous phase II study with a dose-intensive weekly cisplatin schedule for six cycles, we observed a partial response in 5 of 14 patients with pleural mesothelioma.
However, response duration was short (median 6 months). Since oral etoposide may theoretically be synergis-tic to cisplatin, we performed a phase II study with the combination of both drugs. Patients and methods Twenty-five chemo-naive patients with pleural mesothelioma were treated with cisplatin 70 mg/m2 days 1–8–15 and days 29–36–43 in combination with oral etoposide 50 mg days 1–15 and days 29–43. Patients with stable disease, or better, continued treatment with oral etoposide 50 mg/m2/day days 1–21 every 28 days. Results All patients were evaluable for response and toxicity. Complete response was observed in one patient and partial responses in 5 patients (RR% 24%; 95% Cl: 10%–45%) for a median duration of 30 weeks.
Twelve patients had stable disease. The response status never improved during maintenance treatment with oral etoposide. Most patients tolerated the regimen very well. Toxicity was mainly haema-tologic with leukocytopenia causing treatment delays in 8 patients. Ototoxicity grade 1 or 2 was observed in 8 patients, neurotoxicity grade 1 in 9 patients and nephrotoxicity grade 1 in 1 patient. Conclusion Frequently administered cisplatin in combination with oral etoposide has a moderate but definite activity in pleural mesothelioma
One interesting study is called, “Trials in malignant mesothelioma. LCSG 851 and 882. Rusch VW” - Chest. 1994 December 106 (6 Suppl) : 359S-362S - Thoracic Surgery Service, Memorial Sloan-Kettering Cancer Center, New York 10021.
Here is an excerpt: “Abstract - In 1985 the Lung Cancer Study Group (LCSG) initiated clinical trials in malignant pleural mesothelioma because LCSG member institutions had access to large numbers of patients and had significant experience treating this uncommon cancer.
The first trial, LCSG 851, defined the patient population seen by the LCSG, and the feasibility of performing surgical resection by extrapleural pneumonectomy in a multi-institutional setting. Of 83 patients entered on this study from September 1985 to June 1988, only 20 could undergo an extrapleural pneumonectomy, and 3 of 20 patients died postoperatively.
This experience prompted the LCSG to explore combining a potentially less morbid operation, pleurectomy/decortication, with adjuvant therapy. The results of another LCSG trial (LCSG 861) and of a small single institutional pilot study demonstrated the feasibility of intrapleural cisplatin-based chemotherapy, and led to the development of LCSG 882, which combined pleurectomy/decortication with postoperative intrapleural, and subsequent systemic, cisplatin-based chemotherapy.
This study was not completed because of discontinuation of funding for the LCSG. However, a single-institution phase 2 trial of very similar design has subsequently shown the feasibility of this combined modality approach.”
Another study is called, “Extended Surgical Staging for Potentially Resectable Malignant Pleural Mesothelioma” by David C. Rice, MB, BCh, Jeremy J. Erasmus, MD, Craig W. Stevens, MD, PhD, Ara A. Vaporciyan, MD, Judy S. Wu, BS, Anne S. Tsao, MD, Garrett L. Walsh, MD, Stephen G. Swisher, MD, Wayne L. Hofstetter, MD, Nelson G. Ordonez, MD, W. Roy Smythe, MD - Ann Thorac Surg 2005;80:1988-1993 - Department of Thoracic and Cardiovascular Surgery, The University of Texas M.D. Anderson Cancer Center, Houston, Texas.
Here is an excerpt: “BACKGROUND: Extrapleural pneumonectomy for malignant pleural mesothelioma (MPM) is a high-risk procedure, and patients require careful preoperative staging to exclude advanced disease. Computed tomography, magnetic resonance imaging, and positron emission tomography are useful staging modalities, but do not reliably identify contralateral mediastinal involvement or transdiaphragmatic invasion. We evaluated the role of extended surgical staging procedures, which generally includes a combination of laparoscopy, peritoneal lavage, and mediastinoscopy, to more precisely stage patients with MPM.
METHODS: One hundred eighteen patients with MPM, deemed clinically and radiologically resectable, underwent extended surgical staging. Mediastinoscopy was performed in 111 patients, laparoscopy in 109 patients, and peritoneal lavage in 78 patients.
RESULTS: Ten (9.2%) patients had gross evidence of transdiaphragmatic or peritoneal involvement. Peritoneal lavage was positive for metastatic MPM in 2 (2.6%) patients, neither of whom had obvious transdiaphragmatic invasion. Ipsilateral mediastinal nodes contained metastatic tumor in 10 of 62 (16.1%) patients. Contralateral nodes were positive in 4 of 111 (3.6%) patients. Of the patients who underwent biopsy of both ipsilateral and contralateral mediastinal nodes, and who had complete pathologic staging after extrapleural pneumonectomy (n = 46), 14 (30.4%) had N2-positive nodes.
Only 5 of these patients were correctly identified by mediastinoscopy (sensitivity 36%, accuracy 80%). Extended surgical staging identified 16 (13.6%) patients who had contralateral nodal involvement, transdiaphragmatic invasion, or positive peritoneal cytology.
CONCLUSIONS: Extended surgical staging defines an important subset of patients with unresectable MPM not identified by imaging. Because of the potential morbidity associated with extrapleural pneumonectomy, we advocate that extended surgical staging be performed in all patients with MPM before resection.
Another interesting study is called, “Phase II study of a short course of weekly high-dose cisplatin combined with long-term oral etoposide in pleural Mesothelioma” - Oxford Journals Medicine Annals of Oncology Volume 6, Issue 6 Pp. 613-616 - A. S. T. Planting1, M. E. L. van der Burg, S. H. Goey, J. H. M. ScheUens, M. J. van den Bent, M. de Boer-Dennert, G. Stoter1 and J. Verweij.
Here is an excerpt: “Abstract - Background In a previous phase II study with a dose-intensive weekly cisplatin schedule for six cycles, we observed a partial response in 5 of 14 patients with pleural mesothelioma.
However, response duration was short (median 6 months). Since oral etoposide may theoretically be synergis-tic to cisplatin, we performed a phase II study with the combination of both drugs. Patients and methods Twenty-five chemo-naive patients with pleural mesothelioma were treated with cisplatin 70 mg/m2 days 1–8–15 and days 29–36–43 in combination with oral etoposide 50 mg days 1–15 and days 29–43. Patients with stable disease, or better, continued treatment with oral etoposide 50 mg/m2/day days 1–21 every 28 days. Results All patients were evaluable for response and toxicity. Complete response was observed in one patient and partial responses in 5 patients (RR% 24%; 95% Cl: 10%–45%) for a median duration of 30 weeks.
Twelve patients had stable disease. The response status never improved during maintenance treatment with oral etoposide. Most patients tolerated the regimen very well. Toxicity was mainly haema-tologic with leukocytopenia causing treatment delays in 8 patients. Ototoxicity grade 1 or 2 was observed in 8 patients, neurotoxicity grade 1 in 9 patients and nephrotoxicity grade 1 in 1 patient. Conclusion Frequently administered cisplatin in combination with oral etoposide has a moderate but definite activity in pleural mesothelioma
Labels:
Mesothelioma,
treatment
11:54 PM
Immunohistochemistry Does Not Reliably Distinguish Malignant From Benign Hyperplastic Mesothelial Cells
Immunohistochemistry Does Not Reliably Distinguish Malignant From Benign Hyperplastic Mesothelial Cells
One interesting study is called, “Hyperplastic mesothelial cells in lymph nodes: Report of six cases of a benign process that can simulate metastatic involvement by mesothelioma or carcinoma” by Pedram Argani, MD, Juan Rosai, - Volume 29, Issue 4, Pages 339-346 (April 1998). Here is an excerpt: “Abstract - We report six cases of hyperplastic mesothelial cells located in the sinuses of lymph nodes.
All patients but one had a concurrent serosal fluid collection (two pericardial, two pleural, one abdominal) at the time of the lymph node biopsy. All effusions cleared with treatment of the underlying disorder, which included lymphoproliferative processes, congestive heart failure, and inflammatory diseases (Dressler syndrome, vasculitis, and glomerulonephritis).
Four cases were associated with vascular prominence of the involved nodal sinuses, a feature that may reflect the cause of the underlying effusion or support the transient persistence of benign mesothelial cells in lymph nodes. Two cases were characterized by distention of the nodal sinuses by sheets of mitotically active mesothelial cells. The differential diagnosis includes metastatic carcinoma, keratin-positive dendritic cells native to lymph nodes, and metastatic malignant mesothelioma.
Because the latter shares both clinical and morphological features with cases of benign mesothelial cells in lymph nodes, we believe that this distinction may not always be possible in a given biopsy specimen and therefore that careful clinical follow-up is required in such cases.”
Another interesting study is called, “Malignant mesothelioma : Immunohistochemistry and DNA ploidy analysis as methods to differentiate mesothelioma from benign reactive mesothelial cell proliferation and adenocarcinoma in pleural and peritoneal effusions” - 2, Allée du Parc de Brabois F-54514 Vandoeuvre-lès-Nancy Cedex France. Here is an excerpt: “Abstract - Objective.-To determine whether malignant mesotheliomas can be differentiated from adenocarcinomas and benign reactive mesothelial cells in pleural and peritoneal fluids using immunohistochemical analysis in conjunction with DNA ploidy analysis.
Design.-Sixteen cases of malignant mesothelioma, including epithelial, sarcomatous, and biphasic types, were collected. DNA analysis using flow cytometry and/or image analysis was performed on paraffin-embedded tissue from 15 of the mesothelioma cases, as well as on cytospin cell preparations from samples of pleural and peritoneal fluids from cases with either cytologically proven adenocarcinoma (seven cases) or benign reactive mesothelial cells (seven cases). Immunohistochemical studies were done in 15 mesotheliomas, 5 adenocarcinomas, and 4 benign reactive mesothelial cell effusions.
Results.-All malignant mesotheliomas tested (100%) stained positively for prekeratin, whereas stains for carcinoembryonic antigen, B72.3, Leu-M1, and Ber-EP4 were negative. Stains vimentin, epithelial membrane antigen, and CA125 were positive in 75%, 75%, and 25% of cases tested, respectively. Benign reactive mesothelial cell cases stained similarly.
Adenocarcinomas were more likely to react positively with B72.3, Ber-EP4, and carcinoembryonic antigen, and negatively with vimentin. DNA analysis showed that all benign cases were diploid, while all adenocarcinomas were nondiploid. Fifty-three percent of the malignant mesotheliomas were nondiploid. Sensitivity for detection of nondiploidy was greater for image analysis than for flow cytometry (100% vs 75%). Conclusions.-B72.3, Ber-EP4, carcinoembryonic antigen, and vimentin are useful immunohistochemical markers in differentiating malignant mesotheliomas from adenocarcinomas, whereas immunohistochemistry does not reliably distinguish malignant from benign hyperplastic mesothelial cells. The addition of DNA ploidy studies is useful for differentiating the latter two groups.”
Another study is called, “Prognostic value of the serum tumour markers Cyfra 21-1 and tissue polypeptide antigen in malignant Mesothelioma” - Volume 25, Issue 1, Pages 25-32 (July 1999) - International Journal for Lung Cancer. Here is an excerpt: “Abstract - In malignant mesothelioma, survival is claimed to be related to age, duration of symptoms, performance status, histological subtype, stage and platelet count.
However the exact prognostic value of these factors is still a matter of debate. We studied the two cytokeratin markers, Cyfra 21-1 and Tissue polypeptide antigen (TPA) for their significance in predicting survival retrospectively in 52 patients. Cyfra 21-1 and TPA were elevated in 26 (50%) and 30 (58%) patients, respectively, and were highly correlated (r=0.98). Univariate analysis of data from 51 patients, showed a relation with survival for performance status (P=0.010), thoracic pain (P=0.014), platelet count (P=0.027), Cyfra 21-1 (P=0.002) and TPA (P=0.003). Multivariate analysis identified independent prognostic significance for performance status, platelet count and Cyfra 21-1.
In addition to performance status (80) the cytokeratin markers identified patients with good prognosis in a log rank test. Values of Cyfra 21-1 and TPA are significantly correlated.
One interesting study is called, “Hyperplastic mesothelial cells in lymph nodes: Report of six cases of a benign process that can simulate metastatic involvement by mesothelioma or carcinoma” by Pedram Argani, MD, Juan Rosai, - Volume 29, Issue 4, Pages 339-346 (April 1998). Here is an excerpt: “Abstract - We report six cases of hyperplastic mesothelial cells located in the sinuses of lymph nodes.
All patients but one had a concurrent serosal fluid collection (two pericardial, two pleural, one abdominal) at the time of the lymph node biopsy. All effusions cleared with treatment of the underlying disorder, which included lymphoproliferative processes, congestive heart failure, and inflammatory diseases (Dressler syndrome, vasculitis, and glomerulonephritis).
Four cases were associated with vascular prominence of the involved nodal sinuses, a feature that may reflect the cause of the underlying effusion or support the transient persistence of benign mesothelial cells in lymph nodes. Two cases were characterized by distention of the nodal sinuses by sheets of mitotically active mesothelial cells. The differential diagnosis includes metastatic carcinoma, keratin-positive dendritic cells native to lymph nodes, and metastatic malignant mesothelioma.
Because the latter shares both clinical and morphological features with cases of benign mesothelial cells in lymph nodes, we believe that this distinction may not always be possible in a given biopsy specimen and therefore that careful clinical follow-up is required in such cases.”
Another interesting study is called, “Malignant mesothelioma : Immunohistochemistry and DNA ploidy analysis as methods to differentiate mesothelioma from benign reactive mesothelial cell proliferation and adenocarcinoma in pleural and peritoneal effusions” - 2, Allée du Parc de Brabois F-54514 Vandoeuvre-lès-Nancy Cedex France. Here is an excerpt: “Abstract - Objective.-To determine whether malignant mesotheliomas can be differentiated from adenocarcinomas and benign reactive mesothelial cells in pleural and peritoneal fluids using immunohistochemical analysis in conjunction with DNA ploidy analysis.
Design.-Sixteen cases of malignant mesothelioma, including epithelial, sarcomatous, and biphasic types, were collected. DNA analysis using flow cytometry and/or image analysis was performed on paraffin-embedded tissue from 15 of the mesothelioma cases, as well as on cytospin cell preparations from samples of pleural and peritoneal fluids from cases with either cytologically proven adenocarcinoma (seven cases) or benign reactive mesothelial cells (seven cases). Immunohistochemical studies were done in 15 mesotheliomas, 5 adenocarcinomas, and 4 benign reactive mesothelial cell effusions.
Results.-All malignant mesotheliomas tested (100%) stained positively for prekeratin, whereas stains for carcinoembryonic antigen, B72.3, Leu-M1, and Ber-EP4 were negative. Stains vimentin, epithelial membrane antigen, and CA125 were positive in 75%, 75%, and 25% of cases tested, respectively. Benign reactive mesothelial cell cases stained similarly.
Adenocarcinomas were more likely to react positively with B72.3, Ber-EP4, and carcinoembryonic antigen, and negatively with vimentin. DNA analysis showed that all benign cases were diploid, while all adenocarcinomas were nondiploid. Fifty-three percent of the malignant mesotheliomas were nondiploid. Sensitivity for detection of nondiploidy was greater for image analysis than for flow cytometry (100% vs 75%). Conclusions.-B72.3, Ber-EP4, carcinoembryonic antigen, and vimentin are useful immunohistochemical markers in differentiating malignant mesotheliomas from adenocarcinomas, whereas immunohistochemistry does not reliably distinguish malignant from benign hyperplastic mesothelial cells. The addition of DNA ploidy studies is useful for differentiating the latter two groups.”
Another study is called, “Prognostic value of the serum tumour markers Cyfra 21-1 and tissue polypeptide antigen in malignant Mesothelioma” - Volume 25, Issue 1, Pages 25-32 (July 1999) - International Journal for Lung Cancer. Here is an excerpt: “Abstract - In malignant mesothelioma, survival is claimed to be related to age, duration of symptoms, performance status, histological subtype, stage and platelet count.
However the exact prognostic value of these factors is still a matter of debate. We studied the two cytokeratin markers, Cyfra 21-1 and Tissue polypeptide antigen (TPA) for their significance in predicting survival retrospectively in 52 patients. Cyfra 21-1 and TPA were elevated in 26 (50%) and 30 (58%) patients, respectively, and were highly correlated (r=0.98). Univariate analysis of data from 51 patients, showed a relation with survival for performance status (P=0.010), thoracic pain (P=0.014), platelet count (P=0.027), Cyfra 21-1 (P=0.002) and TPA (P=0.003). Multivariate analysis identified independent prognostic significance for performance status, platelet count and Cyfra 21-1.
In addition to performance status (80) the cytokeratin markers identified patients with good prognosis in a log rank test. Values of Cyfra 21-1 and TPA are significantly correlated.
Labels:
Mesothelioma,
treatment
9:17 PM
Mesothelioma And Cancer Gene Therapy
Mesothelioma And Cancer Gene Therapy
One interesting study is called, “Adenovirus-mediated wild-type p53 overexpression reverts tumourigenicity of human mesothelioma cells.” By Giuliano M, Catalano A, Strizzi L, Vianale G, Capogrossi M, Procopio A. Int J Mol Med. 2000 Jun;5(6):591-6. Department of Oncology and Neuroscience, Clinical Pathology Section, Gabriele D'Annunzio University, 66013 Chieti, Italy. Here is an excerpt: “Abstract - Pleural malignant mesothelioma (MM) shows poor survival, regardless of tumour stage at diagnosis. MM is unresponsive to present treatment regimens and new protocols are desperately needed. The localised nature, the potential accessibility, and the relative lack of distant metastases make MM a particularly attractive candidate for somatic gene therapy. A common target for cancer gene therapy is the tumour suppressor protein p53. p53 does not seem to be mutated or deleted in MM, but it can be inactivated by binding to other proteins, like mdm2 and SV40 large T antigen. We tested the effects of a replication-deficient adenoviral vector carrying wild-type p53 cDNA in human MM cells. Our results show that >95% of MM cells were efficiently infected with 25 multiplicity of infection (MOI) of vector. Wild-type p53 was effectively expressed resulting in >80% inhibition of proliferation in MM cells. AdCMV.p53 infection induced apoptosis while controls did not show any evident morphological alterations. Ex vivo p53 gene transfer experiments inhibited tumourigenesis in nude mice. In vivo, direct intratumour injection of AdCMV.p53 arrested tumour growth and prolonged survival of treated mice. These results indicate that p53-gene therapy should be strongly exploited for clinical trials in MM patients.”
Another study is called, “Congenital polycystic tumor of the atrioventricular node (endodermal heterotopia, mesothelioma): A histogenetic appraisal with evidence for its endodermal origin” - Human Pathology Volume 18, Issue 8, August 1987, Pages 791-795 by MD Gerald Fine and MD Usha Raju. Here is an excerpt: “The small, variously designated, primary atrioventricular node tumor has been considered to be of endothelial, endodermal, or mesothelial origin. To identify its derivation, we studied seven tumors using silver staining and immunocytochemical labeling with a variety of antibodies. Cytoplasmic argyrophil granules but not argentaffin granules were found in isolated cells among the more numerous bubule-lining cells in four tumors. Serotonin and calcitonin were demonstrable in seven and six tumors, respectively, in a similar distribution to that of the argyrophil cells. A positive reaction of different distribution from that of the argyrophil cells was noted in a varying number of tubule-lining cells for carcinoembryonic antigen, epithelial membrane antigen, and blood group antigen in seven, four, and seven tumors, respectively. No activity was noted in the tumor cells for factor VIII-related antigen or a number of peptides. An endodermal rather than mesothelial or epithelial origin for the tumor is substantiated by the presence of neuroendocrine cells in the midst of the more numerous carcinoembryonic-antigen-positive lining cells of the tumor tubules.”
Another study is called, “SV40 expression in human neoplastic and non-neoplastic tissues: perspectives on diagnosis, prognosis and therapy of human malignant mesothelioma.” By Procopio A, Marinacci R, Marinetti MR, Strizzi L, Paludi D, Iezzi T, Tassi G, Casalini A, Modesti A. Dev Biol Stand. 1998;94:361-7. Department of Oncology and Neuroscience, Gabriele D'Annunzio University, Chieti, Italy. Here is an excerpt: “Abstract - We have recently demonstrated the association of SV40 and human pleural malignant mesothelioma. Here, we have investigated whether SV40 viral sequences may be associated with other human tumours or other non-neoplastic pathology and whether SV40 DNA or protein expression may be of diagnostic, prognostic or therapeutic relevance. DNA was extracted from paraffin embedded tissues. SV40, JC and BK viral sequences were detected by the polymerase chain reaction and molecular hybridization with specific probes. The screening with three different sets of SV40-related primers demonstrated that 7/18 (38.8%) mesothelioma specimens were SV40 positive as well as 5/18 (27.7%) tubercular pleural lesions. None of the 18 lung cancers, nor the 20 pleural non-specific inflammatory specimens tested were positive. Twenty-five blood samples and 18 urinary sediments from MM patients were also negative. We have also found that SV40 Tag proteins are present in mesothelioma cells and tumours. Tag proteins may interfere with tumour suppressor gene products, such as p53. Preliminary results suggest that wild type p53 transgene expression, obtained after infection with recombinant adenovirus (AdCMV.p53), inhibited in vitro and in vivo proliferation, inducing apoptosis of mesothelioma cells. Infections with control viruses were ineffective. Thus, SV40 DNA and Tag expression in mesothelioma tumour cells, though probably not relevant for diagnostic or prognostic purposes, may be crucial for innovative gene therapy strategies.”
One interesting study is called, “Adenovirus-mediated wild-type p53 overexpression reverts tumourigenicity of human mesothelioma cells.” By Giuliano M, Catalano A, Strizzi L, Vianale G, Capogrossi M, Procopio A. Int J Mol Med. 2000 Jun;5(6):591-6. Department of Oncology and Neuroscience, Clinical Pathology Section, Gabriele D'Annunzio University, 66013 Chieti, Italy. Here is an excerpt: “Abstract - Pleural malignant mesothelioma (MM) shows poor survival, regardless of tumour stage at diagnosis. MM is unresponsive to present treatment regimens and new protocols are desperately needed. The localised nature, the potential accessibility, and the relative lack of distant metastases make MM a particularly attractive candidate for somatic gene therapy. A common target for cancer gene therapy is the tumour suppressor protein p53. p53 does not seem to be mutated or deleted in MM, but it can be inactivated by binding to other proteins, like mdm2 and SV40 large T antigen. We tested the effects of a replication-deficient adenoviral vector carrying wild-type p53 cDNA in human MM cells. Our results show that >95% of MM cells were efficiently infected with 25 multiplicity of infection (MOI) of vector. Wild-type p53 was effectively expressed resulting in >80% inhibition of proliferation in MM cells. AdCMV.p53 infection induced apoptosis while controls did not show any evident morphological alterations. Ex vivo p53 gene transfer experiments inhibited tumourigenesis in nude mice. In vivo, direct intratumour injection of AdCMV.p53 arrested tumour growth and prolonged survival of treated mice. These results indicate that p53-gene therapy should be strongly exploited for clinical trials in MM patients.”
Another study is called, “Congenital polycystic tumor of the atrioventricular node (endodermal heterotopia, mesothelioma): A histogenetic appraisal with evidence for its endodermal origin” - Human Pathology Volume 18, Issue 8, August 1987, Pages 791-795 by MD Gerald Fine and MD Usha Raju. Here is an excerpt: “The small, variously designated, primary atrioventricular node tumor has been considered to be of endothelial, endodermal, or mesothelial origin. To identify its derivation, we studied seven tumors using silver staining and immunocytochemical labeling with a variety of antibodies. Cytoplasmic argyrophil granules but not argentaffin granules were found in isolated cells among the more numerous bubule-lining cells in four tumors. Serotonin and calcitonin were demonstrable in seven and six tumors, respectively, in a similar distribution to that of the argyrophil cells. A positive reaction of different distribution from that of the argyrophil cells was noted in a varying number of tubule-lining cells for carcinoembryonic antigen, epithelial membrane antigen, and blood group antigen in seven, four, and seven tumors, respectively. No activity was noted in the tumor cells for factor VIII-related antigen or a number of peptides. An endodermal rather than mesothelial or epithelial origin for the tumor is substantiated by the presence of neuroendocrine cells in the midst of the more numerous carcinoembryonic-antigen-positive lining cells of the tumor tubules.”
Another study is called, “SV40 expression in human neoplastic and non-neoplastic tissues: perspectives on diagnosis, prognosis and therapy of human malignant mesothelioma.” By Procopio A, Marinacci R, Marinetti MR, Strizzi L, Paludi D, Iezzi T, Tassi G, Casalini A, Modesti A. Dev Biol Stand. 1998;94:361-7. Department of Oncology and Neuroscience, Gabriele D'Annunzio University, Chieti, Italy. Here is an excerpt: “Abstract - We have recently demonstrated the association of SV40 and human pleural malignant mesothelioma. Here, we have investigated whether SV40 viral sequences may be associated with other human tumours or other non-neoplastic pathology and whether SV40 DNA or protein expression may be of diagnostic, prognostic or therapeutic relevance. DNA was extracted from paraffin embedded tissues. SV40, JC and BK viral sequences were detected by the polymerase chain reaction and molecular hybridization with specific probes. The screening with three different sets of SV40-related primers demonstrated that 7/18 (38.8%) mesothelioma specimens were SV40 positive as well as 5/18 (27.7%) tubercular pleural lesions. None of the 18 lung cancers, nor the 20 pleural non-specific inflammatory specimens tested were positive. Twenty-five blood samples and 18 urinary sediments from MM patients were also negative. We have also found that SV40 Tag proteins are present in mesothelioma cells and tumours. Tag proteins may interfere with tumour suppressor gene products, such as p53. Preliminary results suggest that wild type p53 transgene expression, obtained after infection with recombinant adenovirus (AdCMV.p53), inhibited in vitro and in vivo proliferation, inducing apoptosis of mesothelioma cells. Infections with control viruses were ineffective. Thus, SV40 DNA and Tag expression in mesothelioma tumour cells, though probably not relevant for diagnostic or prognostic purposes, may be crucial for innovative gene therapy strategies.”
Labels:
Mesothelioma,
treatment
12:33 AM
Five Common Symptoms Of Mesothelioma
Five Common Symptoms Of Mesothelioma
Mesothelioma is a type of cancer that affects people who have been exposed to asbestos. The time period between the asbestos exposure and the onset of mesothelioma is typically very long. Some people do not develop any mesothelioma symptoms until 40 years or more after the asbestos exposure. This makes it very difficult to diagnose both mesothelioma and asbestosis (another condition caused by asbestos exposure).
Another factor that makes the mesothelioma diagnosis difficult is the variety of mesothelioma types. Mesothelioma develops in the lining of internal organs. Thus, it can affect the lining of the lungs, abdomen, heart and testicles as well as spread to the surrounding tissues. Depending on the exact location of the mesothelioma cancer, the symptoms might vary. The following is a list of five common mesothelioma symptoms.
1. Pain in the Chest and/or Abdomen
Mesothelioma cancer can produce pain in various body parts. The pain becomes stronger as the cancer advances. Pleural mesothelioma (cancer in the lining of the lungs) often causes pain in the chest. In addition, the patient might have difficulty breathing. The shortness of breath might increase as the cancer advances and causes pleural effusion (retention of fluid in the lining of the lungs). Persistent abdominal pain might be a sign of peritoneal mesothelioma (cancer in the lining of the stomach).
2. Coughing
Many patients with pleural mesothelioma experience a persistent, dry cough. As the cancer spreads, they might cough up blood. If you notice any of these symptoms, see your doctor immediately.
3. Unexplained Weight Loss
While most people welcome weight loss as a positive event, large and unexplained weight loss might be a sign of trouble. Such sudden weight loss might be a sign that the body is under extreme pressure produced by cancerous cells and is using internal fatty tissue reserves as a source of energy to fight the disease.
4. Persistent Fatigue
Fatigue is typically a normal bodily response to physical and psychological exhaustion. However, if you feel fatigued all the time for no apparent reason, this might be a sign of cancer. You should see your physician if you feel fatigued even as you wake up after eight or nine hours of sleep.
5. Night Sweats and/or Fever
As mesothelioma spreads, it produces a growing number of cancerous cells, which begin to interfere with basic physiological functions. As a result, internal tissues might begin to swell, and various body cavities might become filled with fluid. The body responds to these occurrences by producing night sweats, which are often accompanied by a low-grade fever. If you experience these symptoms, see your doctor for a thorough medical evaluation.
If you are diagnosed with mesothelioma, your physician will most likely recommend aggressive therapies to slow the spread of cancer and kill off the cancerous cells. Sadly, even with the most advanced cancer therapies, the mesothelioma life expectancy remains less than one year. However, new treatments are being developed, offering mesothelioma patients hope of remission and a longer, more satisfying life.
Mesothelioma is a type of cancer that affects people who have been exposed to asbestos. The time period between the asbestos exposure and the onset of mesothelioma is typically very long. Some people do not develop any mesothelioma symptoms until 40 years or more after the asbestos exposure. This makes it very difficult to diagnose both mesothelioma and asbestosis (another condition caused by asbestos exposure).
Another factor that makes the mesothelioma diagnosis difficult is the variety of mesothelioma types. Mesothelioma develops in the lining of internal organs. Thus, it can affect the lining of the lungs, abdomen, heart and testicles as well as spread to the surrounding tissues. Depending on the exact location of the mesothelioma cancer, the symptoms might vary. The following is a list of five common mesothelioma symptoms.
1. Pain in the Chest and/or Abdomen
Mesothelioma cancer can produce pain in various body parts. The pain becomes stronger as the cancer advances. Pleural mesothelioma (cancer in the lining of the lungs) often causes pain in the chest. In addition, the patient might have difficulty breathing. The shortness of breath might increase as the cancer advances and causes pleural effusion (retention of fluid in the lining of the lungs). Persistent abdominal pain might be a sign of peritoneal mesothelioma (cancer in the lining of the stomach).
2. Coughing
Many patients with pleural mesothelioma experience a persistent, dry cough. As the cancer spreads, they might cough up blood. If you notice any of these symptoms, see your doctor immediately.
3. Unexplained Weight Loss
While most people welcome weight loss as a positive event, large and unexplained weight loss might be a sign of trouble. Such sudden weight loss might be a sign that the body is under extreme pressure produced by cancerous cells and is using internal fatty tissue reserves as a source of energy to fight the disease.
4. Persistent Fatigue
Fatigue is typically a normal bodily response to physical and psychological exhaustion. However, if you feel fatigued all the time for no apparent reason, this might be a sign of cancer. You should see your physician if you feel fatigued even as you wake up after eight or nine hours of sleep.
5. Night Sweats and/or Fever
As mesothelioma spreads, it produces a growing number of cancerous cells, which begin to interfere with basic physiological functions. As a result, internal tissues might begin to swell, and various body cavities might become filled with fluid. The body responds to these occurrences by producing night sweats, which are often accompanied by a low-grade fever. If you experience these symptoms, see your doctor for a thorough medical evaluation.
If you are diagnosed with mesothelioma, your physician will most likely recommend aggressive therapies to slow the spread of cancer and kill off the cancerous cells. Sadly, even with the most advanced cancer therapies, the mesothelioma life expectancy remains less than one year. However, new treatments are being developed, offering mesothelioma patients hope of remission and a longer, more satisfying life.
By: Devin Taylor
Labels:
Mesothelioma,
treatment
12:01 AM
Clinical Trials For Mesothelioma: Who Are Involved, Stages, And Mesothelioma Clinical Trial Reports
Clinical Trials For Mesothelioma: Who Are Involved, Stages, And Mesothelioma Clinical Trial Reports
What is a clinical trial?
A Clinical Trial is a research study done on humans following a very strict protocol. The goal of a clinical trial is to develop new drugs and treatments for all types of diseases, most especially fatal ones such as Mesothelioma.
Before any medicine is considered effective and safe for the general public to take, it has to undergo a thorough process in a clinical trial.
Who are involved in Mesothelioma clinical trials?
The people involved in these biomedical studies are the researcher, who make up the very detailed plan of how the procedure shall be done, the volunteer who will be the subject of the trial, and the review board who usually consists of scientists, oncologists, other physicians, and nurses.
The review board is indirectly involved with the procedures, but it monitors the trial and gives an annual formal review. The volunteers who participate are in most cases, patients diagnosed with Mesothelioma and other types of malignant cancer. Most mesothelioma patients resort to clinical trials as their last hope for a cure.
What are the stages a clinical trial undergoes?
To avoid confusing the term 'stages' with the gravity or extent of the disease, we shall use the term 'phases'.
Generally, a clinical trial has three phases, although a fourth phase is now being considered for the purpose of post-marketing studies. The fourth phase basically checks on the effectiveness of the FDA-approved drug which had already gone through all three phases.
The first phase determines the drug's correct dosage and focuses primarily on safety, rather than the drug's efficacy. The test is done on a small group of 20-80 persons for the first phase.
The second phase verifies if the new drug has a definite effect against a particular disease. This is also where the ideal dosage of the drug is evaluated and the results of the first phase is confirmed. The test is conducted on a larger group of people around 100-300 individuals.
The third phase compares the new drug against the existing standard treatment for a particular disease or illness. The new drug is combined with other drugs to determine side effects, and different doses are tested for the same purpose and to check the efficacy of the drug. This last phase is conducted on a large scale where up to 3,000 people are participants.
Do all Mesothelioma patients have to undergo these clinical trials?
Mesothelioma patients are in no way obliged to participate in biomedical studies and researches. Oncologists may recommend these, especially when patients are considering new types of treatment, but the decision is up to the patient and the patient's family.
Trial reports on Mesothelioma cases raise hope for Mesothelioma patients. The report summarizes the results of the research procedure and is normally published in medical journals for evaluation, and to serve as the basis of continued experimentation by other health professionals.
There are different types of Mesothelioma, would a single successful clinical trial be enough for all types of this disease?
There were Mesothelioma Clinical Trial reports conducted for different types and extent of Mesothelioma. A few examples are the following:
For progressive malignant Pleural Mesothelioma (developed in the lining of the lungs), Phase III Vorinostat trial was conducted where physicians use a chemotherapy drug called Vorinostat to kill cancerous cells and stop the cell's division by blocking enzymes that are needed for the cancerous cells to multiply.
For advanced malignant Mesothelioma, Phase II Pemetrexed Disodium with Gemcitabine is a trial conducted to examine the effects of chemotherapy drugs such as Gemcitabine and Pemetrexed Disodium on recurrent malignant Mesothelioma.
For patients with unresectable malignant Mesothelioma, Phase II AZD2171 clinical trial was conducted so doctors can investigate the use of such chemotherapy drugs for inhibiting enzymes and block the flow of blood into the tumor. The trial was dedicated to help patients suffering from advanced, sarcotamous, epithelial, and recurrent malignant Mesothelioma.
What is a clinical trial?
A Clinical Trial is a research study done on humans following a very strict protocol. The goal of a clinical trial is to develop new drugs and treatments for all types of diseases, most especially fatal ones such as Mesothelioma.
Before any medicine is considered effective and safe for the general public to take, it has to undergo a thorough process in a clinical trial.
Who are involved in Mesothelioma clinical trials?
The people involved in these biomedical studies are the researcher, who make up the very detailed plan of how the procedure shall be done, the volunteer who will be the subject of the trial, and the review board who usually consists of scientists, oncologists, other physicians, and nurses.
The review board is indirectly involved with the procedures, but it monitors the trial and gives an annual formal review. The volunteers who participate are in most cases, patients diagnosed with Mesothelioma and other types of malignant cancer. Most mesothelioma patients resort to clinical trials as their last hope for a cure.
What are the stages a clinical trial undergoes?
To avoid confusing the term 'stages' with the gravity or extent of the disease, we shall use the term 'phases'.
Generally, a clinical trial has three phases, although a fourth phase is now being considered for the purpose of post-marketing studies. The fourth phase basically checks on the effectiveness of the FDA-approved drug which had already gone through all three phases.
The first phase determines the drug's correct dosage and focuses primarily on safety, rather than the drug's efficacy. The test is done on a small group of 20-80 persons for the first phase.
The second phase verifies if the new drug has a definite effect against a particular disease. This is also where the ideal dosage of the drug is evaluated and the results of the first phase is confirmed. The test is conducted on a larger group of people around 100-300 individuals.
The third phase compares the new drug against the existing standard treatment for a particular disease or illness. The new drug is combined with other drugs to determine side effects, and different doses are tested for the same purpose and to check the efficacy of the drug. This last phase is conducted on a large scale where up to 3,000 people are participants.
Do all Mesothelioma patients have to undergo these clinical trials?
Mesothelioma patients are in no way obliged to participate in biomedical studies and researches. Oncologists may recommend these, especially when patients are considering new types of treatment, but the decision is up to the patient and the patient's family.
Trial reports on Mesothelioma cases raise hope for Mesothelioma patients. The report summarizes the results of the research procedure and is normally published in medical journals for evaluation, and to serve as the basis of continued experimentation by other health professionals.
There are different types of Mesothelioma, would a single successful clinical trial be enough for all types of this disease?
There were Mesothelioma Clinical Trial reports conducted for different types and extent of Mesothelioma. A few examples are the following:
For progressive malignant Pleural Mesothelioma (developed in the lining of the lungs), Phase III Vorinostat trial was conducted where physicians use a chemotherapy drug called Vorinostat to kill cancerous cells and stop the cell's division by blocking enzymes that are needed for the cancerous cells to multiply.
For advanced malignant Mesothelioma, Phase II Pemetrexed Disodium with Gemcitabine is a trial conducted to examine the effects of chemotherapy drugs such as Gemcitabine and Pemetrexed Disodium on recurrent malignant Mesothelioma.
For patients with unresectable malignant Mesothelioma, Phase II AZD2171 clinical trial was conducted so doctors can investigate the use of such chemotherapy drugs for inhibiting enzymes and block the flow of blood into the tumor. The trial was dedicated to help patients suffering from advanced, sarcotamous, epithelial, and recurrent malignant Mesothelioma.
By: S.Callaghan
Labels:
Mesothelioma,
treatment
9:14 PM
T-cells the key to curing mesothelioma
T-cells the key to curing mesothelioma and The most effective weapon against mesothelioma
may be inside us—specifically, in our T-cells. Mesothelioma treatment
often relies on chemotherapy and radiation, both of which produce
unpleasant side effects, and some mesothelioma patients are too advanced in terms of the cancer or in terms of age to withstand an invasive surgery.
"Researchers have kept cancer at bay in three patients with chronic lymphocytic leukemia by genetically engineering the patients’ own T-cells to recognize leukemia cell antigens, then kill the cancer cells,” Tia Ghose wrote in yesterday’s The Scientist.
In two studies published in this week’s New England Journal of Medicine and Science Translational Medicine, the focus is on the T-cells’ stunning success against late-stage leukemia. Two of the patients in the study went into a complete remission, and the third had a partial response.
The treatment could potentially be developed to fight not just leukemia, but other cancers as well. Kerry Sheridan wrote for the AFP yesterday
While it remains unknown how long the treatment may keep cancer at bay, researchers were excited to see that "memory" T-cells remained months after the cancer disappeared, indicating the body is retaining some protection.
The next step is to try the technique in two children and at least 13 adults with CD19-positive leukemia.
They are also looking to determine whether the approach could target non-Hodgkin's lymphoma and acute lymphocytic leukemia, mesothelioma cancer cells, ovarian and pancreatic cancer cells.
By using the body’s own T-cells, mesothelioma treatment based off of the positive leukemia results could mean hope for meso patients who are not good candidates for surgery, or are looking for a treatment that does not cause the severe side effects anyone who has been through chemo or radiation knows all too well.
This is fantastic. Although study co-author David Porter, an oncologist at UPenn, said it is "still too early to say [the patients] have been cured," I'm celebrating anyway.
And as one patient said in a statement to the press: "I'm healthy and still in remission. I know this may not be a permanent condition, but I decided to declare victory."
source: http://urdoctor-info.blogspot.com/2013/10/t-cells-key-to-curing-mesothelioma.html
"Researchers have kept cancer at bay in three patients with chronic lymphocytic leukemia by genetically engineering the patients’ own T-cells to recognize leukemia cell antigens, then kill the cancer cells,” Tia Ghose wrote in yesterday’s The Scientist.
In two studies published in this week’s New England Journal of Medicine and Science Translational Medicine, the focus is on the T-cells’ stunning success against late-stage leukemia. Two of the patients in the study went into a complete remission, and the third had a partial response.
The treatment could potentially be developed to fight not just leukemia, but other cancers as well. Kerry Sheridan wrote for the AFP yesterday
While it remains unknown how long the treatment may keep cancer at bay, researchers were excited to see that "memory" T-cells remained months after the cancer disappeared, indicating the body is retaining some protection.
The next step is to try the technique in two children and at least 13 adults with CD19-positive leukemia.
They are also looking to determine whether the approach could target non-Hodgkin's lymphoma and acute lymphocytic leukemia, mesothelioma cancer cells, ovarian and pancreatic cancer cells.
By using the body’s own T-cells, mesothelioma treatment based off of the positive leukemia results could mean hope for meso patients who are not good candidates for surgery, or are looking for a treatment that does not cause the severe side effects anyone who has been through chemo or radiation knows all too well.
This is fantastic. Although study co-author David Porter, an oncologist at UPenn, said it is "still too early to say [the patients] have been cured," I'm celebrating anyway.
And as one patient said in a statement to the press: "I'm healthy and still in remission. I know this may not be a permanent condition, but I decided to declare victory."
source: http://urdoctor-info.blogspot.com/2013/10/t-cells-key-to-curing-mesothelioma.html
Labels:
Mesothelioma,
treatment
9:12 PM
Pericardial mesothelioma
Pericardial mesothelioma affects
the lining surrounding the heart (pericardium). It is the rarest form
of mesothelioma and only accounts for 1% of all diagnoses.
Overview Pericardial Mesothelioma
Pericardial mesothelioma is a cancer which affects the pericardium, which is the lining surrounding the heart. It is currently unknown how the asbestos fibers get into the pericardium. Pericardial mesothelioma is extremely hard to detect. Men are two times more likely to be diagnosed with pericardial mesothelioma than women. There have been cases of pericardial mesothelioma metastasizing to the lung (pleural) or abdomen (peritoneal).
Symptoms Pericardial Mesothelioma
Patients may experience chest pain or other symptoms of pericardial mesothelioma. One of the most common reasons pericardial mesothelioma goes undetected is because it is highly uncommon for mesothelioma to originate in the pericardium. Patients have also reported symptoms that cause it to be mistaken for other heart ailments.
Physicians have a difficult time diagnosing pericardial mesothelioma for many reasons. The extreme rarity of pericardial mesothelioma is the main reason it is difficult to diagnose. It has also been confused with constrictive pericarditis, cardiac tamponade (pressure from fluid buildup) and cardiac failure. However, pericardial mesothelioma can be diagnosed through fluid and tissue biopsies. Patients with pericardial mesothelioma commonly complain about chest pain. When mesothelioma is suspected, cardiac surgeons extract fluid or tissue and test the sample for mesothelioma.
Doctors utilize tests like the echocardiogram and CT scan to gather images that may help conclude if a patient has pericardial mesothelioma. An echocardiogram uses sound waves to diagnose or monitor heart ailments, including atrial fibrillation, heart disease and pericardial mesothelioma. The echo allows a doctor to see how a patient’s heart is beating and pumping blood. Many patients with pericardial mesothelioma experience chest pain because their heart is unable to pump at maximum capacity. Echocardiograms are also essential to determine the extent to which the heart has been affected by the mesothelioma.
Treatment Pericardial Mesothelioma
Treatment options for pericardial mesothelioma are restrictive because of the proximity of the lining to the heart itself. Unlike pleural or peritoneal mesothelioma, where the lung or abdominal lining can be removed, the pericardium is presents further risks and can be difficult to remove.
Pericardiectomy Surgery
Mesothelioma Pericardiectomy SurgeryIf patients are deemed candidates, they may be able to receive a pericardiectomy. A pericardiectomy is the removal of some or all of the pericardium. This procedure is done to relieve the heart from being constricted. It is a risky surgery because of the heart being so close and risk of damage in the process. It’s also a very rare procedure in the case of mesothelioma, as many diagnoses have already metastasized. It is also seldom performed because the diagnoses of pericardial mesothelioma are few and far between. Only 1% of all diagnosed mesothelioma originates in the pericardium.
Prognosis Pericardial Mesothelioma
The prognosis for patients with pericardial mesothelioma is poorer than for pleural and peritoneal mesothelioma. The rarity of this type of mesothelioma means it isn’t able to be studied as much as other mesotheliomas, contributing to the poor prognosis. There is also less information available about how the asbestos fibers lodge into the pericardium and which treatments are most effective. However, some cases show a positive outlook in treatment options. As more cases surface, additional treatment options are in the process of being researched and developed.
One patient who underwent a pericardiectomy survived five years after his initial surgery date. There has been research conducted through Johns Hopkins Hospital that shows pericardiectomies are performed with lower mortality rates as time goes on. Taking part in clinical trials offers unique treatments and is one way many patients improve their prognosis.
source: http://urdoctor-info.blogspot.com/2013/10/pericardial-mesothelioma.html
Overview Pericardial Mesothelioma
Pericardial mesothelioma is a cancer which affects the pericardium, which is the lining surrounding the heart. It is currently unknown how the asbestos fibers get into the pericardium. Pericardial mesothelioma is extremely hard to detect. Men are two times more likely to be diagnosed with pericardial mesothelioma than women. There have been cases of pericardial mesothelioma metastasizing to the lung (pleural) or abdomen (peritoneal).
Symptoms Pericardial Mesothelioma
Patients may experience chest pain or other symptoms of pericardial mesothelioma. One of the most common reasons pericardial mesothelioma goes undetected is because it is highly uncommon for mesothelioma to originate in the pericardium. Patients have also reported symptoms that cause it to be mistaken for other heart ailments.
- Chest Pain
- Shortness of Breath
- Swelling of Face or Arms
- Fatigue
- Cough
- Pericardial Effusion
- Irregular Heartbeat
- Murmurs
Physicians have a difficult time diagnosing pericardial mesothelioma for many reasons. The extreme rarity of pericardial mesothelioma is the main reason it is difficult to diagnose. It has also been confused with constrictive pericarditis, cardiac tamponade (pressure from fluid buildup) and cardiac failure. However, pericardial mesothelioma can be diagnosed through fluid and tissue biopsies. Patients with pericardial mesothelioma commonly complain about chest pain. When mesothelioma is suspected, cardiac surgeons extract fluid or tissue and test the sample for mesothelioma.
Doctors utilize tests like the echocardiogram and CT scan to gather images that may help conclude if a patient has pericardial mesothelioma. An echocardiogram uses sound waves to diagnose or monitor heart ailments, including atrial fibrillation, heart disease and pericardial mesothelioma. The echo allows a doctor to see how a patient’s heart is beating and pumping blood. Many patients with pericardial mesothelioma experience chest pain because their heart is unable to pump at maximum capacity. Echocardiograms are also essential to determine the extent to which the heart has been affected by the mesothelioma.
Treatment Pericardial Mesothelioma
Treatment options for pericardial mesothelioma are restrictive because of the proximity of the lining to the heart itself. Unlike pleural or peritoneal mesothelioma, where the lung or abdominal lining can be removed, the pericardium is presents further risks and can be difficult to remove.
Pericardiectomy Surgery
Mesothelioma Pericardiectomy SurgeryIf patients are deemed candidates, they may be able to receive a pericardiectomy. A pericardiectomy is the removal of some or all of the pericardium. This procedure is done to relieve the heart from being constricted. It is a risky surgery because of the heart being so close and risk of damage in the process. It’s also a very rare procedure in the case of mesothelioma, as many diagnoses have already metastasized. It is also seldom performed because the diagnoses of pericardial mesothelioma are few and far between. Only 1% of all diagnosed mesothelioma originates in the pericardium.
Prognosis Pericardial Mesothelioma
The prognosis for patients with pericardial mesothelioma is poorer than for pleural and peritoneal mesothelioma. The rarity of this type of mesothelioma means it isn’t able to be studied as much as other mesotheliomas, contributing to the poor prognosis. There is also less information available about how the asbestos fibers lodge into the pericardium and which treatments are most effective. However, some cases show a positive outlook in treatment options. As more cases surface, additional treatment options are in the process of being researched and developed.
One patient who underwent a pericardiectomy survived five years after his initial surgery date. There has been research conducted through Johns Hopkins Hospital that shows pericardiectomies are performed with lower mortality rates as time goes on. Taking part in clinical trials offers unique treatments and is one way many patients improve their prognosis.
source: http://urdoctor-info.blogspot.com/2013/10/pericardial-mesothelioma.html
Labels:
Mesothelioma,
treatment
9:09 PM
Peritoneal mesothelioma
Peritoneal mesothelioma is a form of cancer affecting the lining of the stomach (the peritoneum). It is caused by the ingestion of asbestos fibers.
Overview Peritoneal Mesothelioma
Peritoneal mesothelioma accounts for 20% – 25% of all mesothelioma cases. It is the most common diagnosis after pleural mesothelioma. Peritoneal mesothelioma develops after asbestos fibers are ingested. The body attempts to filter and remove these fibers, but sometimes the fibers attach to the peritoneum. Scar tissue builds up as a response to the body’s fight against the irritation of the fibers and can result in genetic cell damage. This can cause unchecked cell division and the formation of a malignant tumor.
Similar to pleural mesothelioma, peritoneal mesothelioma is most common in men who are between the ages of 50-69 years old. Peritoneal mesothelioma does not usually spread to the lymphatic system (lymph nodes) or blood stream. It usually metastasizes in large masses in the same areas where it originated. Learn more about peritoneal mesothelioma treatment options in our free Mesothelioma Guide.
Symptoms Peritoneal MesotheliomaA patient with peritoneal mesothelioma may not experience symptoms at all. If symptoms are demonstrated, they may be mistaken for other illnesses. The earlier the mesothelioma is detected, the sooner it can be treated. One common symptom in many peritoneal mesothelioma patients is the existence of fluid pockets called ascites, which often cause the stomach region to bulge outward.
Diagnosis Peritoneal Mesothelioma
CT scans or MRI test results may not show the presence of peritoneal mesothelioma. Peritoneal tumors that show up on these scans are often confused with abdominal distension (gas). X-rays are the most commonly used imaging tool to diagnose peritoneal mesothelioma because tumors are easier to distinguish from distension. Doctors may also use a technique called peritoneoscopy. In a peritoneoscopy a surgeon makes a small incision in the patient’s abdomen and uses a small camera to explore the abdomen. There is also a tool on the camera that helps to extract tissue on the peritoneum to test for mesothelioma.
Doctors do not use a standard staging system when diagnosing peritoneal mesothelioma. Because the abdomen consists of several organs, peritoneal mesothelioma develops differently in every patient. For this reason, there are several staging systems for this type of mesothelioma, but none have been widely accepted as accurate. Generally, in stage one, the mesothelioma is centralized in the abdomen and is more than likely able to be entirely removed. As it progresses to stage 2, the cancer may spread more but is still contained in the peritoneum. In the third stage, the cancer begins to metastasize to other organs, such as the liver and colon. In the final stage, stage 4, the mesothelioma has spread to other organs outside the abdomen. These stages are extremely variable, making diagnosis difficult and necessitating the need for a mesothelioma specialist.
Treatment Peritoneal Mesothelioma
Treatment options are dependent on the stage a peritoneal mesothelioma patient is diagnosed with. There are more curative treatment options, like cytoreduction surgery, for patients with earlier stages. Patients in the later stages may receive palliative treatments, like radiation or chemotherapy. Another palliative treatment option may be a paracentesis to drain the fluid buildup in the abdomen.
The most successful treatment conducted has been the combination of cytoreduction surgery and HIPEC (hyperthermic intraperitoneal chemotherapy). The cytoreduction removes most of the cancerous tumor and HIPEC has been shown to kill the remaining cells. This treatment has been relatively successful in patients with good general health. Find a peritoneal mesothelioma specialist using our free Doctor Match Program.
Surgery Peritoneal Mesothelioma
 Cytoreduction Surgery
Cytoreduction Surgery
Peritoneal Mesothelioma Cytoreduction Surgery TreatmentCytoreduction is also referred to as “debulking.” The goal of cytoreduction is to remove as much of the tumor as possible, if not all of it. It is often not possible to remove the entire tumor. The peritoneum (lining of the abdomen) is completely removed and is usually performed in patients with stage 1 or 2 peritoneal mesothelioma. It is also done for other abdominal cancers, so it is performed widely. Cytoreduction recovery can take anywhere from 7 to 13 days. One study showed a majority of patients experiencing nausea up to 13 days after their surgery. Regular activities, such as eating, drinking, re-gaining bowel functions, and mobilization were re-established within 11 days after the cytoreduction and HIPEC.
Hyperthermic Intraperitoneal Chemotherapy (HIPEC)
Hyperthermic Intraperitneal Chemotherapy is also known as HIPEC treatment. HIPEC is used in patients who have cancers of the abdomen. This high dose of chemotherapy removes any remaining cancer cells left after a cytoreduction surgery. HIPEC is a heated and sterilized chemotherapy treatment. The side effects of this chemotherapy are less than those of regularly administered chemotherapy. At the end of the 60-90 minutes, the chemotherapy is washed out of the body.
Secondary Treatment Peritoneal Mesothelioma
Chemotherapy
Peritoneal mesothelioma patients in the later stages may receive chemotherapy for palliative purposes. The patients may be given the same combination as with pleural mesothelioma, pemetrexed and cisplatin. Studies are also being done on the effectiveness of the drugs vinorelbine and gemcitabine in combination with cisplatin.
A recent case in 2009 shows promise with the combination of two popular chemotherapy drugs in patients with peritoneal mesothelioma. A patient went in for an unrelated procedure and which signs of peritoneal mesothelioma were found. The patient was given the combination of permetrexed (500 mg) and cisplatin (80 mg). After the first six cycles all signs and markers of the peritoneal mesothelioma were gone. Six months later, CT scans showed no changes or reoccurrence regarding the mesothelioma. Four years later, the patient is alive with no signs of disease progression.
Studies show the normal survival rate of patients with peritoneal mesothelioma is around 7.6 months if they do not receive chemotherapy. Forty-one percent of patients who were given the combination experienced improvement, while 17% showed satisfactory results with cisplatin alone. On average, patients lived 12.1 months longer when having received the combination, compared to 9.3 months on just cisplatin.
Radiation
For many peritoneal mesothelioma patients, radiation is not usually effective. It may shrink tumors before or after a cytoreduction. However, there have been no cases reported of complete eradication by solely using radiation. A mesothelioma specialist can determine if radiation is right for the patient based on their specific diagnosis.
Prognosis Peritoneal Mesothelioma
Although there isn’t currently a cure for mesothelioma, the outlook of new research is hopeful. There have been cases of long-term survivors who have been in remission for over fifteen years. The most successful cases are those whose mesothelioma is detected in the earlier stages and treatment immediately begins. Most cases include a cytoreductive surgery and HIPEC. This method of treatment is responsible for the recovery of survivors Alexis Kidd and Jill Litton.
Although there are similarities between pleural and peritoneal mesothelioma, the treatment options differ. The median survival time for patients who have not had the cytoreductive surgery is about a year; however, in patients who have had the surgery, survival grows up to five years. One study even reported a median survival time of over seven years among participants. Read the incredible stories of people who survived mesothelioma.
source: http://urdoctor-info.blogspot.com/2013/10/peritoneal-mesothelioma.html
Overview Peritoneal Mesothelioma
Peritoneal mesothelioma accounts for 20% – 25% of all mesothelioma cases. It is the most common diagnosis after pleural mesothelioma. Peritoneal mesothelioma develops after asbestos fibers are ingested. The body attempts to filter and remove these fibers, but sometimes the fibers attach to the peritoneum. Scar tissue builds up as a response to the body’s fight against the irritation of the fibers and can result in genetic cell damage. This can cause unchecked cell division and the formation of a malignant tumor.
Similar to pleural mesothelioma, peritoneal mesothelioma is most common in men who are between the ages of 50-69 years old. Peritoneal mesothelioma does not usually spread to the lymphatic system (lymph nodes) or blood stream. It usually metastasizes in large masses in the same areas where it originated. Learn more about peritoneal mesothelioma treatment options in our free Mesothelioma Guide.
Symptoms Peritoneal MesotheliomaA patient with peritoneal mesothelioma may not experience symptoms at all. If symptoms are demonstrated, they may be mistaken for other illnesses. The earlier the mesothelioma is detected, the sooner it can be treated. One common symptom in many peritoneal mesothelioma patients is the existence of fluid pockets called ascites, which often cause the stomach region to bulge outward.
- Abdominal Pain
- Loss of Appetite
- Blood Clots
- Fatigue
- Fluid Buildup (Ascites)
- Nausea
- Abdominal Swelling
- Fever or Sweating
- Tissue Lumps in the Abdomen
- Anemia
- Seizures
- Bowel Problems
Diagnosis Peritoneal Mesothelioma
CT scans or MRI test results may not show the presence of peritoneal mesothelioma. Peritoneal tumors that show up on these scans are often confused with abdominal distension (gas). X-rays are the most commonly used imaging tool to diagnose peritoneal mesothelioma because tumors are easier to distinguish from distension. Doctors may also use a technique called peritoneoscopy. In a peritoneoscopy a surgeon makes a small incision in the patient’s abdomen and uses a small camera to explore the abdomen. There is also a tool on the camera that helps to extract tissue on the peritoneum to test for mesothelioma.
Doctors do not use a standard staging system when diagnosing peritoneal mesothelioma. Because the abdomen consists of several organs, peritoneal mesothelioma develops differently in every patient. For this reason, there are several staging systems for this type of mesothelioma, but none have been widely accepted as accurate. Generally, in stage one, the mesothelioma is centralized in the abdomen and is more than likely able to be entirely removed. As it progresses to stage 2, the cancer may spread more but is still contained in the peritoneum. In the third stage, the cancer begins to metastasize to other organs, such as the liver and colon. In the final stage, stage 4, the mesothelioma has spread to other organs outside the abdomen. These stages are extremely variable, making diagnosis difficult and necessitating the need for a mesothelioma specialist.
Treatment Peritoneal Mesothelioma
Treatment options are dependent on the stage a peritoneal mesothelioma patient is diagnosed with. There are more curative treatment options, like cytoreduction surgery, for patients with earlier stages. Patients in the later stages may receive palliative treatments, like radiation or chemotherapy. Another palliative treatment option may be a paracentesis to drain the fluid buildup in the abdomen.
The most successful treatment conducted has been the combination of cytoreduction surgery and HIPEC (hyperthermic intraperitoneal chemotherapy). The cytoreduction removes most of the cancerous tumor and HIPEC has been shown to kill the remaining cells. This treatment has been relatively successful in patients with good general health. Find a peritoneal mesothelioma specialist using our free Doctor Match Program.
Surgery Peritoneal Mesothelioma
 Cytoreduction Surgery
Cytoreduction SurgeryPeritoneal Mesothelioma Cytoreduction Surgery TreatmentCytoreduction is also referred to as “debulking.” The goal of cytoreduction is to remove as much of the tumor as possible, if not all of it. It is often not possible to remove the entire tumor. The peritoneum (lining of the abdomen) is completely removed and is usually performed in patients with stage 1 or 2 peritoneal mesothelioma. It is also done for other abdominal cancers, so it is performed widely. Cytoreduction recovery can take anywhere from 7 to 13 days. One study showed a majority of patients experiencing nausea up to 13 days after their surgery. Regular activities, such as eating, drinking, re-gaining bowel functions, and mobilization were re-established within 11 days after the cytoreduction and HIPEC.
Hyperthermic Intraperitoneal Chemotherapy (HIPEC)
Hyperthermic Intraperitneal Chemotherapy is also known as HIPEC treatment. HIPEC is used in patients who have cancers of the abdomen. This high dose of chemotherapy removes any remaining cancer cells left after a cytoreduction surgery. HIPEC is a heated and sterilized chemotherapy treatment. The side effects of this chemotherapy are less than those of regularly administered chemotherapy. At the end of the 60-90 minutes, the chemotherapy is washed out of the body.
- Also referred to as “hot chemo”.
- Usually done after cytoreduction.
- Administered both during surgery (most effective) and after using an abdominal catheter.
Secondary Treatment Peritoneal Mesothelioma
Chemotherapy
Peritoneal mesothelioma patients in the later stages may receive chemotherapy for palliative purposes. The patients may be given the same combination as with pleural mesothelioma, pemetrexed and cisplatin. Studies are also being done on the effectiveness of the drugs vinorelbine and gemcitabine in combination with cisplatin.
A recent case in 2009 shows promise with the combination of two popular chemotherapy drugs in patients with peritoneal mesothelioma. A patient went in for an unrelated procedure and which signs of peritoneal mesothelioma were found. The patient was given the combination of permetrexed (500 mg) and cisplatin (80 mg). After the first six cycles all signs and markers of the peritoneal mesothelioma were gone. Six months later, CT scans showed no changes or reoccurrence regarding the mesothelioma. Four years later, the patient is alive with no signs of disease progression.
Studies show the normal survival rate of patients with peritoneal mesothelioma is around 7.6 months if they do not receive chemotherapy. Forty-one percent of patients who were given the combination experienced improvement, while 17% showed satisfactory results with cisplatin alone. On average, patients lived 12.1 months longer when having received the combination, compared to 9.3 months on just cisplatin.
Radiation
For many peritoneal mesothelioma patients, radiation is not usually effective. It may shrink tumors before or after a cytoreduction. However, there have been no cases reported of complete eradication by solely using radiation. A mesothelioma specialist can determine if radiation is right for the patient based on their specific diagnosis.
Prognosis Peritoneal Mesothelioma
Although there isn’t currently a cure for mesothelioma, the outlook of new research is hopeful. There have been cases of long-term survivors who have been in remission for over fifteen years. The most successful cases are those whose mesothelioma is detected in the earlier stages and treatment immediately begins. Most cases include a cytoreductive surgery and HIPEC. This method of treatment is responsible for the recovery of survivors Alexis Kidd and Jill Litton.
Although there are similarities between pleural and peritoneal mesothelioma, the treatment options differ. The median survival time for patients who have not had the cytoreductive surgery is about a year; however, in patients who have had the surgery, survival grows up to five years. One study even reported a median survival time of over seven years among participants. Read the incredible stories of people who survived mesothelioma.
source: http://urdoctor-info.blogspot.com/2013/10/peritoneal-mesothelioma.html
Labels:
Mesothelioma,
treatment
9:01 PM
Pleural Mesothelioma
Pleural Mesothelioma is a form of cancer in the pleura (protective lining of the lung). It is caused by exposure to asbestos fibers.
Overview Pleural Mesothelioma
Pleural mesothelioma is the most common form of mesothelioma and makes up 75% of all mesothelioma diagnoses. It develops when asbestos fibers are inhaled and attach to the lining of the lungs, known as the pleura. This can include both the visceral (inner) or the parietal (outer) pleura. The particles irritate the pleura, resulting in inflammation. The pleural tissue develops into scar tissue, which can cause genetic damage and tumors. It takes anywhere from ten to fifty years after asbestos exposure for mesothelioma to develop in the pleura.
Mesothelioma in the pleura spreads quickly because of its proximity to vital organs. Generally, it develops in the lining of the lungs and then spreads to the rest of the lung, the chest wall, or the nearby diaphragm. The central location of the lungs in the body means the other vital organs are nearby.
Mesothelioma in the pleural space can metastasize to the lymph nodes, which can cause cancer to spread throughout the body more quickly. It is common for it to metastasize to the central organs. There have also been cases which linked pleural mesothelioma to spread to the brain, although this is uncommon.
Fighting pleural mesothelioma takes a mix of information an action. Our free Mesothelioma Guide puts the power in your hands to find a top pleural mesothelioma specialist as well as which treatment options work best.
Symptoms Pleural Mesothelioma
Prior to a pleural mesothelioma diagnosis, patients may experience symptoms associated with common illnesses, such as the onset of a fever, shortness of breath or coughing. Although these symptoms are common, if a patient has been exposed to asbestos in the past, it is important they consult a physician.
Causes Pleural Mesothelioma
The main cause of mesothelioma is exposure to asbestos fibers. Asbestos products are usually found in homes and businesses built prior to the 1980’s. Occupational exposure is the most common form, although exposure in the home can occur as well. Genetic factors may also play a role in the development of mesothelioma. However, this connection has not been fully investigated. The genetic links may actually be sourced to common exposure to asbestos-related environments.
Veterans with Mesothelioma
The largest group diagnosed with mesothelioma are military veterans, specifically Navy service members. Asbestos was commonly used because of its flame-resistant qualities. Millions of veterans were exposed between the years 1930 and 1980. Veterans diagnosed with mesothelioma can work with our team (including a retired Lieutenant Commander) to get help filing a VA Claim. There are options available for those who served our country.
Diagnosis Pleural Mesothelioma
If test results determine the possible presence of cancerous tumors or growths, doctors perform a biopsy on the area. A biopsy is a small fluid or tissue sample that determines if cancer cells are present. Tissue biopsies are the most reliable, with a 96% conclusivity. Depending on the results of the biopsy and if the cancer has spread, a patient is diagnosed with a specific stage of pleural mesothelioma. The stages range from 1 to 4.
The 4 Stages:
Treatment Debate of Pleural Mesothelioma
Treatment Options for pleural mesothelioma are dependent upon which stage a patient is diagnosed with. Patients with earlier stages of pleural mesothelioma are usually candidates for curative surgeries like an extrapleural pneumonectomy or a pleurectomy. Patients who are in the later stages of mesothelioma may receive more palliative treatment options, such as a pleurodesis, to help alleviate the discomfort caused by the tumors.
There is a current debate between the effectiveness of an extrapleural pneumonectomy (EPP) versus a pleurectomy. The EPP surgery was initially developed for mesothelioma by Dr. David Sugarbaker at Brigham and Women’s Hospital in Boston, MA. An EPP removes the entire lung, part of the pericardium, and part of the diaphragm – all the areas the mesothelioma has metastasized to during advanced stage 2 mesothelioma. There have been many successful EPP surgeries. Patients’ survival rate dramatically increases and there have been cases of patients living over fifteen years after having the EPP surgery.
Dr. Robert Cameron is the original developer of the pleurectomy surgery and is the most outspoken critic of the extrapleural pneumonectomy. He has stated that the pleurectomy is the better surgery for patients because it is a lung sparing surgery with lower mortality rates. A pleurectomy may sometimes include removal of part of the lung, but not the entire lung. Rarely does a pleurectomy remove all the affected areas of stage 2 pleural mesothelioma due to the intricate spread. According to him, the quality of life of a pleurectomy patient is better than one who had an extrapleural pneumontectomy. Although the pleurectomy has a lower mortality rate, treatment plans may involve different surgical procedures depending on the patient’s unique diagnosis.
Since finding a doctor is one of the most critical steps a patient can take, we developed a resource to assist with it. Our free Doctor Match program connects patients with pleural mesothelioma specialists across the nation. We’ve built relationships across the country with the very best mesothelioma specialists and place patients with a doctor who is best able to treat them.
Surgery Extrapleural Pneumonectomy (EPP)
Extrapleural Pneumonectomy Mesothelioma Surgery TreatmentExtrapleural pneumonectomy is the most common surgical treatment for stage 1 or 2 malignant pleural mesothelioma. During EPP, a surgeon removes the diseased lung as well as the pleural space covering the lung, heart, and diaphragm.
The goal of EPP is to remove as much, if not all, of the cancerous tissue possible. Chemotherapy may be used as a pre-surgery (neoadjuvant) precaution to shrink the tumors and may also be recommended post-surgery (adjuvant). Dr. David Sugarbaker, of Brigham & Women’s Hospital, is the creator of the EPP and is one of the leading mesothelioma physicians in the country.
Pleurectomy/Decortication (P/D)
Pleurectomy with Decortication Mesothelioma Surgery TreatmentPleurectomy with decortication may be used in stage 1 mesothelioma to remove the cancerous pleura. It also may be used in stages 3 or 4 to alleviate pain while breathing because the lung cannot expand entirely.
Pleurectomy with decortication helps patients ease in breathing and controls the fluid build-up that generally happens in the pleural space. Tumors on the surface of the lung are also removed. Palliative surgeries are done to relieve any pain the patient may be experiencing and improve their quality of life.
Secondary Treatments Pleural Mesothelioma
Chemotherapy
Currently, the most effective form of chemotherapy given to pleural mesothelioma patients is the combination of pemetrexed (Alimta) and cisplatin (Platinol). This combination is the standard for chemotherapy treatment and is given to all pleural mesothelioma patients. Pemetrexed is the only medication of its kind approved by the FDA to specifically treat mesothelioma. Doctors may also use drugs not yet been approved to treat mesothelioma patients.
Another form of chemotherapy given to pleural mesothelioma patients is known as intrapleural chemotherapy. This process involves a catheter which applies the chemotherapy directly to the tumor site. This technique is only used in stage 1 patients because the cancer has only spread to the pleura.
Radiation
For mesothelioma patients, radiation techniques are rarely curative when used on their own. Radiation may be used before or after surgery, such as an extrapleural pnuemonectomy. Radiation used after surgery has shown to greatly reduce the possibility of cancer recurrence.
Radiation is not usually used in the later stages of pleural mesothelioma because it has spread to other parts of the body. The only instance in which radiation would be used would be for palliative purposes. There may be chest discomfort due to fluid build up or tumor pressure, in these circumstances, radiation may be used. The radiation may help with tumor pressure because it shrinks the tumor to alleviate the pain.
Patients looking for a complete pleural mesothelioma treatment plan (including chemotherapy and radiation treatments) should visit Cancer Center Guide
Prognosis
There are many factors that play a role in a patient’s prognosis. The cell type, stage, age, and overall health of the patients are all important. In pleural mesothelioma cases women have a better survival rate than men.
One study done by Dr. David Sugarbaker showed there was a five year (or more) survival rate in patients diagnosed with pleural mesothelioma. These patients had epithelioid cell types and no lymph node involvement (stage 1). The patients underwent an extrapleural pneumonectomy which removed most of the cancer cells. The outlook of treating pleural mesothelioma is getting brighter as more research is being done.
Rarely does a pleurectomy remove all the affected areas of stage 2 pleural mesothelioma due to the intricate spread. Early treatment is key in the prognosis of mesothelioma. The earlier the cancer is detected, the sooner treatment can begin. Patients who are fighting pleural mesothelioma can learn a lot from mesothelioma survivors. Their stories of hope prove that its possible to live beyond a prognosis.
source: http://urdoctor-info.blogspot.com/2013/10/pleural-mesothelioma.html
Overview Pleural Mesothelioma
Pleural mesothelioma is the most common form of mesothelioma and makes up 75% of all mesothelioma diagnoses. It develops when asbestos fibers are inhaled and attach to the lining of the lungs, known as the pleura. This can include both the visceral (inner) or the parietal (outer) pleura. The particles irritate the pleura, resulting in inflammation. The pleural tissue develops into scar tissue, which can cause genetic damage and tumors. It takes anywhere from ten to fifty years after asbestos exposure for mesothelioma to develop in the pleura.
Mesothelioma in the pleura spreads quickly because of its proximity to vital organs. Generally, it develops in the lining of the lungs and then spreads to the rest of the lung, the chest wall, or the nearby diaphragm. The central location of the lungs in the body means the other vital organs are nearby.
Mesothelioma in the pleural space can metastasize to the lymph nodes, which can cause cancer to spread throughout the body more quickly. It is common for it to metastasize to the central organs. There have also been cases which linked pleural mesothelioma to spread to the brain, although this is uncommon.
Fighting pleural mesothelioma takes a mix of information an action. Our free Mesothelioma Guide puts the power in your hands to find a top pleural mesothelioma specialist as well as which treatment options work best.
Symptoms Pleural Mesothelioma
Prior to a pleural mesothelioma diagnosis, patients may experience symptoms associated with common illnesses, such as the onset of a fever, shortness of breath or coughing. Although these symptoms are common, if a patient has been exposed to asbestos in the past, it is important they consult a physician.
- Lower Back Pain
- Shortness of Breath (dyspnea)
- Unexplained Weight Loss
- Swelling of Face or Arms
- Fluid Buildup (Pleural Effusion)
- Chest Pain (Pleurisy)
- Dry or Painful Cough
- Fever or Sweating
- Tissue Lumps in the Chest
- Coughing up Blood (Hemoptysis)
Causes Pleural Mesothelioma
The main cause of mesothelioma is exposure to asbestos fibers. Asbestos products are usually found in homes and businesses built prior to the 1980’s. Occupational exposure is the most common form, although exposure in the home can occur as well. Genetic factors may also play a role in the development of mesothelioma. However, this connection has not been fully investigated. The genetic links may actually be sourced to common exposure to asbestos-related environments.
Veterans with Mesothelioma
The largest group diagnosed with mesothelioma are military veterans, specifically Navy service members. Asbestos was commonly used because of its flame-resistant qualities. Millions of veterans were exposed between the years 1930 and 1980. Veterans diagnosed with mesothelioma can work with our team (including a retired Lieutenant Commander) to get help filing a VA Claim. There are options available for those who served our country.
Diagnosis Pleural Mesothelioma
If test results determine the possible presence of cancerous tumors or growths, doctors perform a biopsy on the area. A biopsy is a small fluid or tissue sample that determines if cancer cells are present. Tissue biopsies are the most reliable, with a 96% conclusivity. Depending on the results of the biopsy and if the cancer has spread, a patient is diagnosed with a specific stage of pleural mesothelioma. The stages range from 1 to 4.
The 4 Stages:
- Stage 1
- The cancer is only located in the pleural lining of the lungs.
- Stage 2
- The cancer has spread to more of the lung, part of the diaphragm, and localized lymph nodes.
- Stage 3
- The cancer has metastasized to nearby organs and mroe lymph nodes
- Stage 4
- The cancer has spread to the other organs and all lymph nodes are fully involved.
Treatment Debate of Pleural Mesothelioma
Treatment Options for pleural mesothelioma are dependent upon which stage a patient is diagnosed with. Patients with earlier stages of pleural mesothelioma are usually candidates for curative surgeries like an extrapleural pneumonectomy or a pleurectomy. Patients who are in the later stages of mesothelioma may receive more palliative treatment options, such as a pleurodesis, to help alleviate the discomfort caused by the tumors.
There is a current debate between the effectiveness of an extrapleural pneumonectomy (EPP) versus a pleurectomy. The EPP surgery was initially developed for mesothelioma by Dr. David Sugarbaker at Brigham and Women’s Hospital in Boston, MA. An EPP removes the entire lung, part of the pericardium, and part of the diaphragm – all the areas the mesothelioma has metastasized to during advanced stage 2 mesothelioma. There have been many successful EPP surgeries. Patients’ survival rate dramatically increases and there have been cases of patients living over fifteen years after having the EPP surgery.
Dr. Robert Cameron is the original developer of the pleurectomy surgery and is the most outspoken critic of the extrapleural pneumonectomy. He has stated that the pleurectomy is the better surgery for patients because it is a lung sparing surgery with lower mortality rates. A pleurectomy may sometimes include removal of part of the lung, but not the entire lung. Rarely does a pleurectomy remove all the affected areas of stage 2 pleural mesothelioma due to the intricate spread. According to him, the quality of life of a pleurectomy patient is better than one who had an extrapleural pneumontectomy. Although the pleurectomy has a lower mortality rate, treatment plans may involve different surgical procedures depending on the patient’s unique diagnosis.
Since finding a doctor is one of the most critical steps a patient can take, we developed a resource to assist with it. Our free Doctor Match program connects patients with pleural mesothelioma specialists across the nation. We’ve built relationships across the country with the very best mesothelioma specialists and place patients with a doctor who is best able to treat them.
Surgery Extrapleural Pneumonectomy (EPP)
Extrapleural Pneumonectomy Mesothelioma Surgery TreatmentExtrapleural pneumonectomy is the most common surgical treatment for stage 1 or 2 malignant pleural mesothelioma. During EPP, a surgeon removes the diseased lung as well as the pleural space covering the lung, heart, and diaphragm.
The goal of EPP is to remove as much, if not all, of the cancerous tissue possible. Chemotherapy may be used as a pre-surgery (neoadjuvant) precaution to shrink the tumors and may also be recommended post-surgery (adjuvant). Dr. David Sugarbaker, of Brigham & Women’s Hospital, is the creator of the EPP and is one of the leading mesothelioma physicians in the country.
Pleurectomy/Decortication (P/D)
Pleurectomy with Decortication Mesothelioma Surgery TreatmentPleurectomy with decortication may be used in stage 1 mesothelioma to remove the cancerous pleura. It also may be used in stages 3 or 4 to alleviate pain while breathing because the lung cannot expand entirely.
Pleurectomy with decortication helps patients ease in breathing and controls the fluid build-up that generally happens in the pleural space. Tumors on the surface of the lung are also removed. Palliative surgeries are done to relieve any pain the patient may be experiencing and improve their quality of life.
Secondary Treatments Pleural Mesothelioma
Chemotherapy
Currently, the most effective form of chemotherapy given to pleural mesothelioma patients is the combination of pemetrexed (Alimta) and cisplatin (Platinol). This combination is the standard for chemotherapy treatment and is given to all pleural mesothelioma patients. Pemetrexed is the only medication of its kind approved by the FDA to specifically treat mesothelioma. Doctors may also use drugs not yet been approved to treat mesothelioma patients.
Another form of chemotherapy given to pleural mesothelioma patients is known as intrapleural chemotherapy. This process involves a catheter which applies the chemotherapy directly to the tumor site. This technique is only used in stage 1 patients because the cancer has only spread to the pleura.
Radiation
For mesothelioma patients, radiation techniques are rarely curative when used on their own. Radiation may be used before or after surgery, such as an extrapleural pnuemonectomy. Radiation used after surgery has shown to greatly reduce the possibility of cancer recurrence.
Radiation is not usually used in the later stages of pleural mesothelioma because it has spread to other parts of the body. The only instance in which radiation would be used would be for palliative purposes. There may be chest discomfort due to fluid build up or tumor pressure, in these circumstances, radiation may be used. The radiation may help with tumor pressure because it shrinks the tumor to alleviate the pain.
Patients looking for a complete pleural mesothelioma treatment plan (including chemotherapy and radiation treatments) should visit Cancer Center Guide
Prognosis
There are many factors that play a role in a patient’s prognosis. The cell type, stage, age, and overall health of the patients are all important. In pleural mesothelioma cases women have a better survival rate than men.
One study done by Dr. David Sugarbaker showed there was a five year (or more) survival rate in patients diagnosed with pleural mesothelioma. These patients had epithelioid cell types and no lymph node involvement (stage 1). The patients underwent an extrapleural pneumonectomy which removed most of the cancer cells. The outlook of treating pleural mesothelioma is getting brighter as more research is being done.
Rarely does a pleurectomy remove all the affected areas of stage 2 pleural mesothelioma due to the intricate spread. Early treatment is key in the prognosis of mesothelioma. The earlier the cancer is detected, the sooner treatment can begin. Patients who are fighting pleural mesothelioma can learn a lot from mesothelioma survivors. Their stories of hope prove that its possible to live beyond a prognosis.
source: http://urdoctor-info.blogspot.com/2013/10/pleural-mesothelioma.html
Labels:
Mesothelioma,
treatment